Veins of the Head and Neck

Veins of the Head and Neck (Internal & External Jugular) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript Notes ☆ Member Only Go to PDF Notes Illustrations ☆ Member Only Go to Illustrations 12345678910 Veins of the Head and Neck – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 Which tributary of the internal jugular vein forms the common facial vein? A) Anterior division of retromandibular vein B) Posterior division of retromandibular vein C) Lingual vein D) Maxillary vein The anterior division of the retromandibular vein forms the common facial vein by joining the facial vein. 2 / 10 Which vein connects intracranial and extracranial venous systems? A) Facial vein B) Retromandibular vein C) Lingual vein D) Common facial vein The facial vein connects intracranial and extracranial systems via the ophthalmic veins. 3 / 10 Which superficial vein is at risk of air embolism during injury? A) Internal jugular vein B) Anterior jugular vein C) External jugular vein D) Vertebral vein The external jugular vein is superficial and at risk for air embolism if severed. 4 / 10 Which vein forms from the confluence of the maxillary and superficial temporal veins? A) External jugular vein B) Posterior auricular vein C) Facial vein D) Retromandibular vein The retromandibular vein is formed by the confluence of the maxillary and superficial temporal veins. 5 / 10 Which tributary of the external jugular vein drains the lateral cervical region? A) Occipital vein B) Transverse cervical vein C) Anterior jugular vein D) Suprascapular vein The transverse cervical vein drains the lateral cervical region into the external jugular vein. 6 / 10 Which vein drains the cavernous sinus into the internal jugular vein? A) Inferior petrosal sinus B) External jugular vein C) Transverse sinus D) Superior petrosal sinus The inferior petrosal sinus drains the cavernous sinus into the internal jugular vein. 7 / 10 What is the termination point of the internal jugular vein? A) Subclavian vein B) Transverse cervical vein C) External jugular vein D) Venous angle The internal jugular vein terminates at the venous angle, forming the brachiocephalic vein. 8 / 10 Which vein directly communicates with the cavernous sinus, facilitating infection spread? A) Ophthalmic veins B) Lingual vein C) Retromandibular vein D) External jugular vein The ophthalmic veins connect the facial vein with the cavernous sinus, allowing infection spread. 9 / 10 Which vein drains the parietal and temporal regions of the scalp? A) Maxillary vein B) Posterior auricular vein C) Superficial temporal vein D) Occipital vein The superficial temporal vein drains the parietal and temporal regions into the retromandibular vein. 10 / 10 What connects the left and right anterior jugular veins in the suprasternal space? A) Transverse cervical vein B) Jugular venous arch C) Retromandibular vein D) Vertebral venous plexus The jugular venous arch connects the left and right anterior jugular veins in the suprasternal space. Your score is The average score is 0% Description This video covers the External Veins of the Head and Face, focusing on the External Jugular Vein and Internal Jugular Vein. Through a detailed schematic, it illustrates their course, tributaries, and drainage. Introduction: The venous system consists of four parts: Veins of the heart Vena Cava Superior Vena Cava Inferior Portal System Venous tributaries are smaller veins that drain into larger veins. The Superior Vena Cava divides into two Brachiocephalic Veins. The Brachiocephalic Vein is formed by the Internal Jugular Vein and the Subclavian Vein. The External Jugular Vein empties into the Subclavian Vein. Veins of the Head: Internal Jugular Vein (Vena Jugularis Interna) Drains from the Sigmoid Sinus (Sinus Sigmoideus). Tributaries: Lingual Vein (V. Lingualis): Dorsal Lingual Vein (Vena Dorsalis Linguae) Deep Lingual Vein (Vena Profunda Linguae) Sublingual Vein (Vena Sublingualis) Common Facial Vein: Facial Vein (Vena Facialis): Deep Facial Vein (Vena Facialis Profunda) drains into the Pterygoid Plexus (Plexus Pterygoideus). The Pterygoid Plexus continues as the Maxillary Vein (Vena Maxillaris). The Maxillary Vein connects with the Retromandibular Vein (Vena Retromandibularis) to form the Superficial Temporal Vein (Vena Temporalis Superficialis). The Superficial Temporal Vein supplies the parietal and frontal regions. The Anterior Root of the Retromandibular Vein connects with the Posterior Root to form the Retromandibular Vein. External Jugular Vein (Vena Jugularis Externa) Formed by the Posterior Root of the Retromandibular Vein and the Posterior Auricular Vein (Vena Auricularis Posterior). Occipital Vein (Vena Occipitalis) – Variations: May drain into the Posterior Auricular Vein, forming the Posterior Root of the External Jugular Vein. May drain directly into the Internal Jugular Vein. Veins of the Neck: Mnemonic for Internal Jugular Vein Tributaries: Medical Schools Let Confident People In M: Middle Thyroid Vein (Vena Thyroidea Media) S: Superior Thyroid Vein (Vena Thyroidea Superior) L: Lingual Vein (Vena Lingualis) C: Common Facial Vein P: Pharyngeal Vein (Vena Pharyngea) – drains the Pharyngeal Plexus I: Inferior Petrosal Sinus (Sinus Petrosus Inferior) Mnemonic for External Jugular Vein Tributaries: PAST P: Posterior External Jugular Vein A: Anterior Jugular Vein (Vena Jugularis Anterior) – forms the Jugular Venous Arch S: Suprascapular Vein (Vena Suprascapularis) T: Transverse Cervical Vein (Vv. Transversae Colli) Clinical Relevance: Jugular Venous Distension (JVD): Can indicate increased right atrial pressure, often seen in heart failure. Facial Vein Connection with Cavernous Sinus: The Deep Facial Vein connects to the Pterygoid Venous Plexus, which communicates with the Cavernous Sinus, posing a risk for infections spreading from the face to the brain (cavernous sinus thrombosis). Internal Jugular Vein Puncture: Common site for central venous catheterization. Sources Used: Memorix Anatomy (2nd Edition) – Hudák Radovan, Kachlík David, Volný Ondřej. Complete Anatomy by 3D4Medical. Biorender. University Notes and Lectures. Transcript Introduction0:00hello and welcome to another video in0:01this video we’re going to look at the0:03veins of the head and neck or to be0:05specific the external veins of the head0:08and the veins of the neck that drain0:10directly into the external and the0:12internal jugler veins and at the end of0:15this
Superior Vena Cava
Superior Vena Cava (Azygos, Hemiazygos, Brachiocephalic) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript Notes ☆ Member Only Go to PDF Notes Illustrations ☆ Member Only Go to Illustrations 12345678910 Superior Vena Cava – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 Which vein receives drainage from the superior intercostal veins on the right? A) Superior phrenic vein B) Internal thoracic vein C) Azygos vein D) Accessory hemiazygos vein The azygos vein receives drainage from the right superior intercostal veins. 2 / 10 What is the relationship of the superior vena cava to the right lung root? A) Posterior B) Medial C) Anterior D) Lateral The superior vena cava lies anterior to the right lung root in the superior mediastinum. 3 / 10 What is the diameter of the superior vena cava? A) 3-4 cm B) 1-2 cm C) 4-5 cm D) 2-3 cm The superior vena cava has a diameter of 2-3 cm. 4 / 10 Which vein is located posterior to the superior vena cava? A) Pericardial veins B) Thymic vein C) Right lung root D) Aortic arch The right lung root lies posterior to the superior vena cava. 5 / 10 Which vein directly drains into the superior vena cava and serves as a collateral pathway for venous return? A) Azygos vein B) Internal jugular vein C) Hemiazygos vein D) Brachiocephalic vein The azygos vein drains into the superior vena cava and provides a collateral pathway for venous return from the thoracic wall. 6 / 10 What is the length of the superior vena cava? A) 5 cm B) 7 cm C) 8 cm D) 6 cm The superior vena cava is approximately 7 cm long. 7 / 10 Which vein drains the esophagus and contributes to the azygos system? A) Pericardial veins B) Mediastinal veins C) Esophageal veins D) Bronchial veins The esophageal veins drain the esophagus and connect to the azygos system. 8 / 10 What is the clinical relevance of the azygos vein during inferior vena cava obstruction? A) Supplies the diaphragm B) Collateral circulation pathway C) Drains lymph nodes D) Drains the pericardium The azygos vein serves as an alternative pathway for venous blood return when the inferior vena cava is obstructed. 9 / 10 What clinical condition is caused by obstruction of the superior vena cava? A) Aortic dissection B) Superior vena cava syndrome (SVCS) C) Pulmonary embolism D) Inferior vena cava syndrome Superior vena cava syndrome results from obstruction or compression, leading to swelling of the face, neck, and upper limbs along with cyanosis. 10 / 10 What vein joins the superior vena cava by draining the posterior thoracic and abdominal walls? A) Mediastinal veins B) Pericardial veins C) Hemiazygos vein D) Azygos vein The azygos vein drains the posterior thoracic and abdominal walls and directly connects to the superior vena cava. Your score is The average score is 0% Description This video covers the Superior Vena Cava, Azygos Vein, Right and Left Brachiocephalic Veins, and their tributaries, with anatomical details and clinical relevance. Superior Vena Cava (V. Cava Superior) Short Vein with a large diameter (2-3 cm). No valves. Azygos Vein (V. Azygos) Unpaired vein located behind the Inferior Vena Cava, on the right side of the vertebral column. Receives blood from the Right Ascending Lumbar Vein (V. Lumbalis Ascendens Dexter). May function as portocaval and cavo-caval anastomoses. Tributaries of Azygos Vein: Visceral Tributaries: Esophageal Veins (Vv. Oesophageales). Bronchial Veins (Vv. Bronchiales). Pericardial Veins (Vv. Pericardiacae). Mediastinal Veins (Vv. Mediastinales). Parietal Tributaries: Hemiazygos Vein (V. Hemiazygos). Accessory Hemiazygos Vein (V. Hemiazygos Accessoria). Right Superior Intercostal Veins (Vv. Intercostales Superior Dextrae). Right Posterior Intercostal Veins (Vv. Intercostales Posteriores Dexter). Superior Phrenic Vein (Vv. Phrenicae Superiores). Left Thoracic Veins: Left Posterior Intercostal Veins (Vv. Intercostales Posteriores Sinistrae), draining into the Accessory Hemiazygos Vein and the Hemiazygos Vein. Right Brachiocephalic Vein (V. Brachiocephalica Dexter) Formed by the union of the Subclavian Vein (V. Subclavia) and the Internal Jugular Vein (V. Jugularis Interna). Approximately 3 cm long. Tributaries of the Right Brachiocephalic Vein: Right Vertebral Vein (V. Vertebralis). Right Inferior Thyroid Vein (V. Thyroidea Inferior Dexter). Right Internal Thoracic Vein (V. Thoracica Interna Dexter). Anterior Intercostal Veins (Vv. Intercostales Anteriores) communicate with the posterior intercostal veins. Musculophrenic Vein (V. Musculophrenica). Superior Epigastric Vein (V. Epigastrica Superior). Right Supreme Intercostal Vein (V. Intercostalis Suprema). Left Brachiocephalic Vein (V. Brachiocephalica Sinister) Approximately 6 cm long. Tributaries of the Left Brachiocephalic Vein: Left Vertebral Vein (V. Vertebralis Sinister). Left Inferior Thyroid Vein (V. Thyroidea Inferior Sinister). Left Internal Thoracic Vein (V. Thoracica Interna Sinister). Left Supreme Intercostal Vein (V. Intercostalis Suprema Sinister). Left Superior Intercostal Vein (V. Intercostalis Superior Sinistra). Thymic Veins (Vv. Thymicae). Pericardiophrenic Veins (V. Pericardiophrenicae). Clinical Relevance: Superior Vena Cava Syndrome (SVCS): Compression or obstruction of the SVC leads to venous congestion, facial swelling, and distended neck veins. Azygos System as a Collateral Pathway: Can compensate for venous return when the IVC or SVC is obstructed. Portocaval Anastomoses: In cases of portal hypertension, azygos tributaries may enlarge, causing esophageal varices. Sources Used: Memorix Anatomy (2nd Edition) – Hudák Radovan, Kachlík David, Volný Ondřej. Complete Anatomy by 3D4Medical. Biorender. University Notes and Lectures. Transcript Introduction0:03Let’s now talk about the superior vena cava and its associated veins.0:07So in this video, we’re first going to talk briefly about the superior vena cava,0:12We’ll talk a little bit about the azygos vein Then we’ll cover the hemiazygos vein and the0:17accessory hemiazygos vein After that, we’ll talk about the right and0:21the left brachiocephalic veins.0:23We’ll go through their characteristics, their tributaries and what structures they all generally0:28drain.Veins of the Systemic Circulation0:29Awesome So, the easiest way to understand the veins0:33of the systemic circulation is to divide them into their own systems.0:37So the veins of the heart form their own system We have the Veins of the Inferior Vena Cava,0:43which is responsible for supplying the
Tibial Arteries
Anterior & Posterior Tibial Arteries Scheme (Course, Branches) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript Notes ☆ Member Only Go to PDF Notes Illustrations ☆ Member Only Go to Illustrations 12345678910 Tibial Arteries – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 Which artery passes through the interosseous membrane to enter the anterior compartment of the leg? A) Peroneal (fibular) artery B) Dorsalis pedis artery C) Posterior tibial artery D) Anterior tibial artery The anterior tibial artery passes through the interosseous membrane to enter the anterior compartment of the leg. 2 / 10 Which artery gives rise to the perforating arteries on the dorsum of the foot? A) Dorsalis pedis artery B) Medial plantar artery C) Posterior tibial artery D) Arcuate artery The arcuate artery gives rise to the perforating arteries on the dorsum of the foot. 3 / 10 Which artery gives rise to the deep plantar artery? A) Lateral plantar artery B) Medial plantar artery C) Dorsalis pedis artery D) Posterior tibial artery The dorsalis pedis artery gives rise to the deep plantar artery, which contributes to the deep plantar arch. 4 / 10 Which branch of the posterior tibial artery supplies the lateral malleolus? A) Lateral malleolar arteries B) Calcaneal arteries C) Arcuate artery D) Medial malleolar artery The lateral malleolar arteries, branches of the peroneal artery, supply the lateral malleolus. 5 / 10 Which artery supplies the lateral compartment of the leg and arises from the posterior tibial artery? A) Anterior tibial artery B) Posterior tibial artery C) Peroneal (fibular) artery D) Dorsalis pedis artery The peroneal (fibular) artery arises from the posterior tibial artery and supplies the lateral compartment of the leg. 6 / 10 Which artery gives rise to the lateral tarsal artery? A) Dorsalis pedis artery B) Medial plantar artery C) Posterior tibial artery D) Anterior tibial artery The dorsalis pedis artery gives rise to the lateral tarsal artery, which supplies the lateral side of the foot. 7 / 10 Which artery supplies the plantar surface of the first toe? A) Dorsalis pedis artery B) Lateral plantar artery C) Arcuate artery D) Medial plantar artery The medial plantar artery supplies the plantar surface of the first toe. 8 / 10 Which artery continues as the dorsalis pedis artery at the level of the ankle joint? A) Posterior tibial artery B) Anterior tibial artery C) Peroneal (fibular) artery D) Lateral plantar artery The anterior tibial artery continues as the dorsalis pedis artery at the level of the ankle joint. 9 / 10 Which branch of the posterior tibial artery supplies the medial ankle region? A) Medial malleolar arteries B) Arcuate artery C) Calcaneal arteries D) Lateral malleolar artery The medial malleolar arteries are branches of the posterior tibial artery and supply the medial ankle region. 10 / 10 Which branch of the anterior tibial artery contributes to the ankle joint’s lateral collateral circulation? A) Anterior medial malleolar artery B) Anterior lateral malleolar artery C) Posterior tibial artery D) Circumflex fibular branch The anterior lateral malleolar artery contributes to the lateral collateral circulation of the ankle joint. Your score is The average score is 0% Description This video covers the Posterior Tibial Artery, Anterior Tibial Artery, and the Blood Supply of the Foot, including key branches and clinical relevance. Posterior Tibial Artery (A. Tibialis Posterior): Circumflex Fibular Artery (R. Circumflexus Fibularis): Contributes to the anastomoses around the knee. Fibular/Peroneal Artery (A. Fibularis/A. Peronea): Major lateral branch supplying the posterior and lateral compartments of the leg. Lateral Malleolar Arteries (Rr. Malleolares Laterales): Supplies the lateral malleolus. Medial Malleolar Arteries (Rr. Malleolares Mediales): Supplies the medial malleolus. Calcaneal Arteries (Rr. Calcanei): Supplies the heel. Lateral Plantar Artery (A. Plantaris Lateralis): Supplies the lateral part of the sole and contributes to the deep plantar arch. Medial Plantar Artery (A. Plantaris Medialis): Supplies the medial part of the sole and first toe. Anterior Tibial Artery (A. Tibialis Anterior): Posterior Tibial Recurrent Artery (A. Recurrens Tibialis Posterior): Anastomoses with genicular arteries. Anterior Tibial Recurrent Artery (A. Recurrens Tibialis Anterior): Contributes to the knee joint supply. Anterior Lateral Malleolar Artery (A. Malleolaris Anterior Lateralis): Supplies the lateral ankle. Anterior Medial Malleolar Artery (A. Malleolaris Anterior Medialis): Supplies the medial ankle. Dorsalis Pedis Artery (A. Dorsalis Pedis): Terminal branch that supplies the dorsum of the foot. Blood Supply of the Foot: Dorsalis Pedis Artery: Lateral Tarsal Artery (A. Tarsalis Lateralis): Supplies lateral dorsum of the foot. Medial Tarsal Arteries (Aa. Tarsales Mediales): Supplies medial dorsum of the foot. Arcuate Artery (A. Arcuata): Forms an arch, giving rise to dorsal metatarsal arteries. Dorsal Metatarsal Arteries (Aa. Metatarsales Dorsales): Each divides into two dorsal digital arteries. 1st Dorsal Metatarsal Artery (A. Metatarsalis Dorsalis Prima): Divides into three dorsal digital arteries. Deep Plantar Artery (A. Plantaris Profunda): Contributes to the deep plantar arch. Plantar Circulation: Lateral Plantar Artery: Forms the Deep Plantar Arch (Arcus Plantaris Pedis) by connecting with the deep plantar artery from dorsalis pedis. Plantar Metatarsal Arteries: Supply toes by dividing into plantar digital arteries. Medial Plantar Artery: Primarily supplies the first toe. Clinical Relevance: Peripheral Arterial Disease (PAD): Commonly affects tibial arteries, leading to ischemia and ulcers. Pulses for Circulatory Assessment: Posterior Tibial Pulse: Palpated behind the medial malleolus. Dorsalis Pedis Pulse: Palpated on the dorsum of the foot. Diabetic Foot Ulcers: Often result from impaired circulation in the plantar arch. Sources Used: Memorix Anatomy (2nd Edition) – Hudák Radovan, Kachlík David, Volný Ondřej. Complete Anatomy by 3D4Medical. Biorender. University Notes and Lectures. Transcript Introduction0:00in this video we’re going to look at the0:02anterior and the posterior tibial0:04arteries0:05as well as the arterial blood supply of0:07the foot and ankle0:08and to do that we first need to look at0:10the posterior aspect of the knee0:12because as the femoral artery comes down0:15it becomes the popliteal artery in the0:17popliteal fossa0:19where it branches out supplying the knee0:21with blood0:22then in front of
Popliteal Artery
Popliteal Artery Scheme (Course, Branches, Patellar Network) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript Notes ☆ Member Only Go to PDF Notes Illustrations ☆ Member Only Go to Illustrations 12345678910 Popliteal Artery – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 Which branch of the popliteal artery is involved in the patellar network and arises from the circumflex fibular artery? A) Inferior medial genicular artery B) Superior lateral genicular artery C) Circumflex fibular branch D) Superior medial genicular artery The circumflex fibular branch contributes to the collateral circulation around the knee joint as part of the patellar network. 2 / 10 Which branch of the popliteal artery provides the main blood supply to the cruciate ligaments? A) Sural arteries B) Middle genicular artery C) Inferior medial genicular artery D) Superior lateral genicular artery The middle genicular artery supplies the cruciate ligaments of the knee joint. 3 / 10 Which genicular artery supplies the medial superior aspect of the knee? A) Superior lateral genicular artery B) Inferior medial genicular artery C) Inferior lateral genicular artery D) Superior medial genicular artery The superior medial genicular artery supplies the medial superior aspect of the knee. 4 / 10 Which branch of the anterior tibial artery contributes to the patellar network? A) Circumflex fibular branch B) Anterior recurrent tibial artery C) Inferior medial genicular artery D) Superior medial genicular artery The anterior recurrent tibial artery, a branch of the anterior tibial artery, contributes to the patellar network. 5 / 10 What is the terminal continuation of the popliteal artery at the lower border of the popliteus muscle? A) Middle genicular artery B) Sural arteries C) Genicular arteries D) Anterior and posterior tibial arteries The popliteal artery terminates as the anterior tibial and posterior tibial arteries at the lower border of the popliteus muscle. 6 / 10 Which branch of the popliteal artery supplies the posterior compartment of the leg? A) Middle genicular artery B) Inferior lateral genicular artery C) Inferior medial genicular artery D) Sural arteries The sural arteries, branches of the popliteal artery, supply the posterior compartment of the leg. 7 / 10 Which artery supplies the superior lateral aspect of the knee? A) Superior lateral genicular artery B) Superior medial genicular artery C) Inferior lateral genicular artery D) Middle genicular artery The superior lateral genicular artery supplies the superior lateral aspect of the knee and contributes to the patellar network. 8 / 10 Which artery in the patellar network is a branch of the anterior tibial artery? A) Circumflex fibular branch B) Sural arteries C) Anterior recurrent tibial artery D) Middle genicular artery The anterior and posterior recurrent tibial arteries, branches of the anterior tibial artery, contribute to the patellar network. 9 / 10 Which branch of the popliteal artery supplies the superior lateral region of the knee joint? A) Middle genicular artery B) Superior lateral genicular artery C) Sural arteries D) Inferior medial genicular artery The superior lateral genicular artery supplies the superior lateral region of the knee joint. 10 / 10 At which anatomical location does the popliteal artery divide into its terminal branches? A) Popliteus muscle B) Popliteal fossa C) Adductor canal D) Femoral triangle The popliteal artery divides into the tibialis anterior and posterior arteries at the level of the popliteus muscle. Your score is The average score is 0% Description This video covers the Popliteal Artery (A. Poplitea), including its course, side branches, and its contribution to the blood supply of the knee through the Patellar Network (Rete Articulare Genu). Course of the Popliteal Artery: Direct continuation of the Femoral Artery after passing through the Adductor Hiatus. Runs superficially in the Popliteal Fossa, deep to the popliteal vein and tibial nerve. Terminates by dividing into two terminal branches: Anterior Tibial Artery (A. Tibialis Anterior): Supplies the anterior compartment of the leg. Posterior Tibial Artery (A. Tibialis Posterior): Supplies the posterior compartment of the leg. Side Branches of the Popliteal Artery: Superior Medial Genicular Artery (A. Superior Medialis Genus): Supplies the medial knee joint. Superior Lateral Genicular Artery (A. Superior Lateralis Genus): Supplies the lateral knee joint. Inferior Medial Genicular Artery (A. Inferior Medialis Genus): Supplies the medial aspect of the inferior knee joint. Inferior Lateral Genicular Artery (A. Inferior Lateralis Genus): Supplies the lateral aspect of the inferior knee joint. Middle Genicular Artery (A. Media Genus): Pierces the knee joint capsule and supplies the cruciate ligaments and synovial membrane. Sural Arteries (Aa. Surales): Supplies the gastrocnemius, soleus, and plantaris muscles. Patellar Network (Rete Articulare Genu) – Blood Supply of the Knee: Descending Genicular Artery (A. Descendens Genus): Branch of the femoral artery. Saphenous Branch: Runs with the saphenous nerve. Muscular and Articular Branches: Supply the knee joint. Descending Branch of Lateral Femoral Circumflex Artery: From the deep femoral artery, contributes to anastomoses around the knee. Posterior and Anterior Recurrent Tibial Arteries: Branches of the anterior tibial artery, supplying the knee joint. Circumflex Fibular Branch: Arises from the posterior tibial artery and contributes to knee vascularization. Clinical Relevance: Popliteal Aneurysm: Most common aneurysm of the peripheral arteries, can compress the tibial nerve causing pain and weakness. Knee Trauma: The popliteal artery is at risk in posterior knee dislocations. Peripheral Arterial Disease (PAD): Can affect the popliteal artery, reducing blood flow to the lower limb. Sources Used: Memorix Anatomy (2nd Edition) – Hudák Radovan, Kachlík David, Volný Ondřej. Complete Anatomy by 3D4Medical. Biorender. University Notes and Lectures. Transcript Introduction0:00hello and welcome to another video in0:01this video we’re going to look at the0:03popliteal artery and the patellar0:05network0:06now the popliteal artery is a direct0:09continuation of the femoral artery0:11so if we now follow the femoral artery0:13and look from this perspective0:15behind the knee you will see that the0:17artery runs very superficially through0:19the popliteal fossa0:20to the popliteal muscle where it ends by0:23dividing into two terminal branches0:26and these are the anterior and the0:28posterior tibial arteriesSide Branches of
Femoral Artery
Femoral Artery Scheme (Course, Branches) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript Notes ☆ Member Only Go to PDF Notes Illustrations ☆ Member Only Go to Illustrations 12345678910 Femoral Artery – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 At which anatomical location does the femoral artery exit the adductor canal? A) Adductor hiatus B) Inguinal ligament C) Popliteal fossa D) Femoral triangle The femoral artery exits the adductor canal through the adductor hiatus to continue as the popliteal artery. 2 / 10 Which branch of the femoral artery supplies the vastus medialis and anastomoses around the knee? A) Superficial epigastric artery B) Profunda femoris artery C) Lateral circumflex femoral artery D) Descending genicular artery The descending genicular artery supplies the vastus medialis and contributes to the arterial anastomoses around the knee. 3 / 10 Which branch of the profunda femoris artery perforates the adductor magnus to supply the posterior compartment of the thigh? A) Superficial epigastric artery B) Lateral circumflex femoral artery C) Perforating arteries D) Medial circumflex femoral artery The perforating arteries of the profunda femoris artery supply the posterior compartment of the thigh. 4 / 10 Which branch of the femoral artery anastomoses with branches of the internal iliac artery around the hip joint? A) External pudendal artery B) Lateral circumflex femoral artery C) Superficial circumflex iliac artery D) Medial circumflex femoral artery The medial circumflex femoral artery anastomoses with branches of the internal iliac artery around the hip joint. 5 / 10 Which artery supplies the skin of the scrotum or labia in the external genitalia? A) Superficial circumflex iliac artery B) Superficial epigastric artery C) External pudendal artery D) Descending genicular artery The external pudendal artery supplies the skin of the scrotum or labia in the external genitalia. 6 / 10 Which branch of the femoral artery supplies the skin of the lower abdomen and upper thigh? A) Descending genicular artery B) External pudendal artery C) Superficial circumflex iliac artery D) Lateral circumflex femoral artery The superficial circumflex iliac artery supplies the skin of the lower abdomen and upper thigh. 7 / 10 What is the terminal branch of the femoral artery after it passes through the adductor hiatus? A) Profunda femoris artery B) Popliteal artery C) Lateral circumflex femoral artery D) Descending genicular artery The popliteal artery is the terminal continuation of the femoral artery after it exits the adductor hiatus. 8 / 10 Which branch of the femoral artery provides the main blood supply to the posterior compartment of the thigh? A) Profunda femoris artery B) External pudendal artery C) Superficial circumflex iliac artery D) Descending genicular artery The profunda femoris artery (deep femoral artery) is the primary blood supply to the posterior thigh compartment. 9 / 10 Which structure forms the medial border of the femoral triangle? A) Pectineus muscle B) Adductor longus C) Iliopsoas muscle D) Sartorius muscle The adductor longus muscle forms the medial border of the femoral triangle. 10 / 10 Which branch of the femoral artery supplies the external genitalia? A) Profunda femoris artery B) Superficial circumflex iliac artery C) External pudendal artery D) Superficial epigastric artery The external pudendal artery arises medially from the femoral artery and supplies the external genitalia. Your score is The average score is 0% Description This video covers the anatomy, course, and side branches of the Femoral Artery (A. Femoralis), a major artery supplying the lower limb. Course of the Femoral Artery: Passes through the Vascular Space (Lacuna Vasorum). Enters the Femoral Triangle, which is bordered by: Sartorius (lateral border) Adductor Longus (medial border) Iliopsoas and Pectineus (floor of the triangle) Travels within the Adductor Canal (Hunter’s Canal). Exits the canal behind the knee via the Adductor Hiatus, becoming the Popliteal Artery (A. Poplitea). Side Branches of the Femoral Artery: Superficial Branches: Superficial Circumflex Iliac Artery (A. Circumflexa Ilium Superficialis): Supplies the superficial inguinal region. Superficial Epigastric Artery (A. Epigastrica Superficialis): Supplies the lower abdominal wall. External Pudendal Artery (Aa. Pudendae Externae): Supplies the external genitalia. Deep Branches: Deep Femoral Artery (A. Profunda Femoris): The main branch supplying deep structures of the thigh. Perforating Arteries (Aa. Perforantes): Pierce the adductor muscles and supply the posterior compartment of the thigh. Lateral Circumflex Femoral Artery (A. Circumflexa Femoris Lateralis): Divides into: Ascending Branch: Supplies the anterior hip region. Transverse Branch: Contributes to the cruciate anastomosis. Descending Branch: Supplies the lateral thigh and knee. Medial Femoral Circumflex Artery (A. Circumflexa Femoris Medialis): Important for blood supply to the femoral head. Descending Genicular Artery (A. Descendens Genus): Supplies the knee joint and surrounding structures. Clinical Relevance: Femoral Pulse: Easily palpable in the femoral triangle, used for clinical assessments. Femoral Artery Cannulation: Common site for catheterization procedures. Avascular Necrosis Risk: Damage to the Medial Femoral Circumflex Artery can lead to femoral head necrosis. Sources Used: Memorix Anatomy (2nd Edition) – Hudák Radovan, Kachlík David, Volný Ondřej. Complete Anatomy by 3D4Medical. Biorender. University Notes and Lectures. Transcript Introduction0:00hello and welcome to another video in0:01this video we’re going to look at the0:03femoral artery0:04now the femoral artery is a large artery0:06in the thigh0:07and the main arterial blood supply to0:09the thigh and the leg0:11it enters the thigh from behind the0:13inguinal ligament0:14in a canal called the vascular space or0:16the lacuna vasodium in latin0:18and guess the name the femoral artery0:20only after it passes the vascular0:22space so first i’ll try to cover the0:25course of this artery as in0:27where it starts and ends and then i’ll0:30cover the branchesCourse0:31now as it passes the vascular space it0:35enters the femoral triangle0:37and here’s a better representation of it0:39the thermal triangle0:40is formed by the sartorius muscle and0:42the adductor longus0:44and within the canal you will find the0:46femoral artery0:48passing between the pectineus and the0:50iliopsoas muscles0:52and so this is the femoral triangle as0:55the femoral artery is relatively0:57superficial within the femoral triangle0:59the femoral pulse is usually easily1:01palpated1:02and if the pulse is diminished this is1:05this may1:05may indicate
Internal Iliac Artery
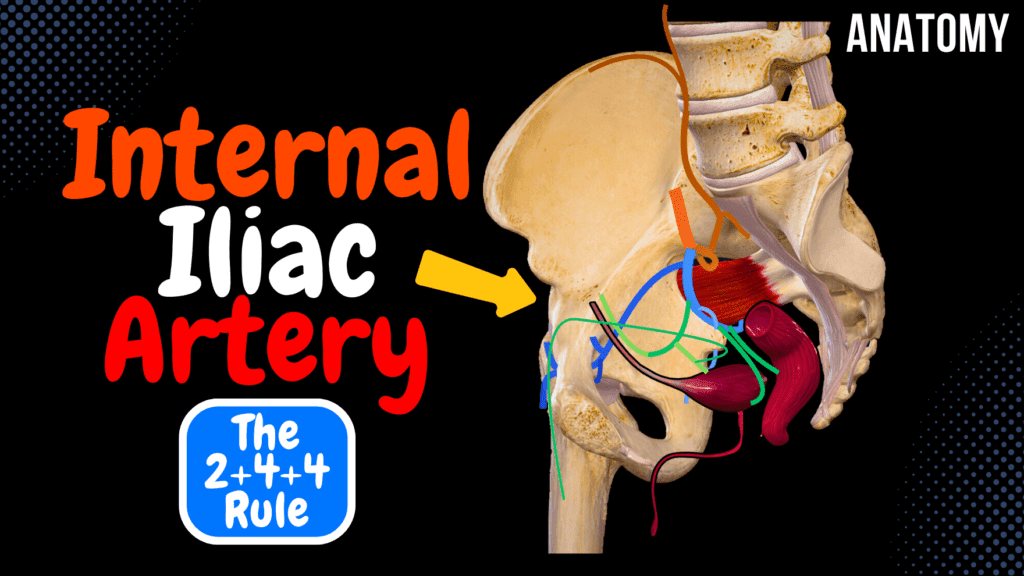
Internal Iliac Artery Scheme (Course, Branches, Mnemonic) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript Notes ☆ Member Only Go to PDF Notes Illustrations ☆ Member Only Go to Illustrations 12345678910 Internal Iliac Artery – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 Which branch of the internal iliac artery supplies the ligament of the femoral head? A) Pubic branch B) Lumbar branch C) Iliac branch D) Acetabular branch The acetabular branch of the obturator artery runs through the ligament of the femoral head to supply the femoral head. 2 / 10 Which artery terminates as the dorsal artery of the penis or clitoris? A) Uterine artery B) Obturator artery C) Inferior gluteal artery D) Internal pudendal artery The internal pudendal artery terminates as the dorsal artery of the penis or clitoris. 3 / 10 Which artery forms the medial umbilical ligament after obliteration postnatally? A) Umbilical artery B) Superior vesical artery C) Middle rectal artery D) Inferior vesical artery The umbilical artery becomes obliterated after birth and forms the medial umbilical ligament. 4 / 10 Which artery provides the superior vesical artery as one of its branches? A) Inferior vesical artery B) Umbilical artery C) Middle rectal artery D) Lateral sacral artery The umbilical artery gives rise to the superior vesical artery before becoming obliterated. 5 / 10 Which artery supplies the perineum and terminates as the dorsal artery of the penis or clitoris? A) Obturator artery B) Internal pudendal artery C) Inferior gluteal artery D) Uterine artery The internal pudendal artery supplies the perineum and terminates as the dorsal artery of the penis or clitoris. 6 / 10 Which branch of the obturator artery supplies the femoral head? A) Pubic branch B) Lumbar branch C) Iliac branch D) Acetabular branch The acetabular branch of the obturator artery passes through the ligament of the femoral head to supply the femoral head. 7 / 10 Which branch of the internal iliac artery supplies the uterus and forms an anastomosis with the ovarian artery? A) Inferior vesical artery B) Umbilical artery C) Middle rectal artery D) Uterine artery The uterine artery supplies the uterus and forms an anastomosis with the ovarian artery from the abdominal aorta. 8 / 10 Which artery contributes to the blood supply of the sacral spinal canal? A) Iliolumbar artery B) Lateral sacral artery C) Middle rectal artery D) Obturator artery The lateral sacral artery gives spinal branches to the sacral spinal canal. 9 / 10 Which branch of the internal iliac artery gives rise to the superior vesical artery? A) Inferior vesical artery B) Middle rectal artery C) Obturator artery D) Umbilical artery The umbilical artery gives rise to the superior vesical artery before becoming obliterated as the medial umbilical ligament. 10 / 10 Which branch of the internal iliac artery supplies the inferior portion of the bladder in males? A) Inferior vesical artery B) Umbilical artery C) Superior vesical artery D) Middle rectal artery The inferior vesical artery supplies the inferior portion of the bladder, prostate, and seminal vesicles in males. Your score is The average score is 0% Description This video covers an easy way to remember the side branches of the Internal Iliac Artery (A. Iliaca Interna) using the 2+4+4 mnemonic. Understanding these branches is crucial for anatomy, surgery, and clinical relevance. Mnemonic: 2+4+4 2 Arteries to the Back Body Wall: Iliolumbar Artery (A. Iliolumbalis): Divides into the Lumbar branch (R. Lumbalis) and Iliac branch (R. Iliacus). Lateral Sacral Artery (A. Sacrales Laterales): Gives off spinal branches (Rr. Spinales), which supply the sacral vertebrae and meninges. 4 Arteries Leaving the Pelvic Cavity: Obturator Artery (A. Obturatoria): Passes through the obturator canal and divides into anterior and posterior branches. Side Branches: Pubic Branch (R. Pubicus): Communicates with the pubic branch of the inferior epigastric artery, forming the Corona Mortis (important in surgery due to risk of excessive bleeding). Acetabular Branch (R. Acetabularis): Runs through the ligament of the femoral head to supply Caput Femoris. Superior Gluteal Artery (A. Glutea Superior): Leaves the pelvis above the Piriformis muscle through the greater sciatic foramen. Inferior Gluteal Artery (A. Glutea Inferior): Leaves the pelvis below the Piriformis muscle. Internal Pudendal Artery (A. Pudenda Interna): Leaves below the Piriformis muscle and travels between the perineal and pelvic diaphragm muscles. Terminates as: Deep and Dorsal Arteries of the Penis (A. Dorsalis Penis & A. Profunda Penis) or the Deep and Dorsal Arteries of the Clitoris (A. Dorsalis Clitoridis & A. Profunda Clitoridis). Side Branches: Inferior Rectal Artery (A. Rectalis Inferior): Supplies the anal canal. Perineal Artery (A. Perinealis): Gives off: Posterior Scrotal Artery (Rr. Scrotales Posteriores) in males. Posterior Labial Artery (Rr. Labiales Posteriores) in females. Urethral Branch (A. Urethralis): Supplies the urethra. Artery of the Bulb of the Penis (A. Bulbi Penis) or Artery of the Bulb of the Vestibule (A. Bulbi Vestibuli) in females. 4 Arteries Staying Inside the Pelvic Cavity: Umbilical Artery (A. Umbilicalis): Partially obliterated after birth, forming the Medial Umbilical Fold (Plica Umbilicalis Medialis). Remaining Part: Superior Vesical Artery (Aa. Vesicales Superiores): Supplies the bladder. Artery of the Ductus Deferens (A. Ductus Deferentis): Supplies the vas deferens, with branches to the urethra. Inferior Vesical Artery (Aa. Vesicales Inferiores): Supplies the lower bladder, prostate, and seminal vesicles (present in males). Uterine Artery (A. Uterina): Runs along the uterus and divides into: Tubal Branch (R. Tubarius): Supplies the Fallopian Tube and Mesosalpinx. Ovarian Branch (R. Ovaricus): Communicates with the Ovarian Artery from the abdominal aorta. Middle Rectal Artery (A. Rectalis Media): Supplies the middle part of the rectum and anastomoses with the superior and inferior rectal arteries. Blood Supply of the Rectum: Superior Rectal Artery: From the Inferior Mesenteric Artery (IMA). Middle Rectal Artery: From the Internal Iliac Artery. Inferior Rectal Artery: From the Internal Pudendal Artery. Clinical Relevance: Corona Mortis: Surgeons must be cautious of the anastomosis between
External Iliac Artery
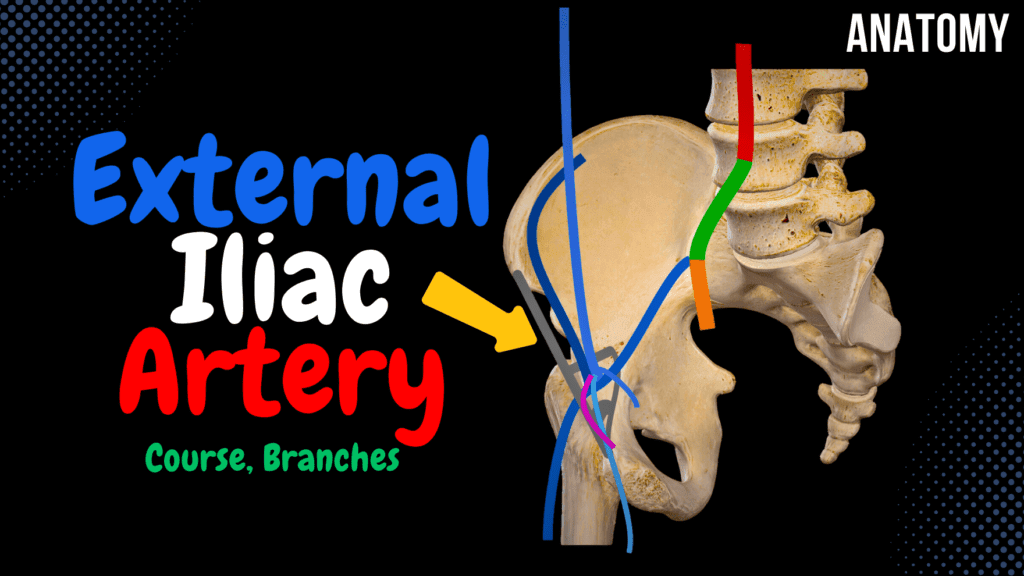
External Iliac Artery Scheme (Course, Branches) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript Notes ☆ Member Only Go to PDF Notes Illustrations ☆ Member Only Go to Illustrations 12345678910 External Iliac Artery – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 Which artery supplies the lower portion of the rectus abdominis muscle? A) Inferior epigastric artery B) Superior epigastric artery C) Deep circumflex iliac artery D) Umbilical artery The inferior epigastric artery supplies the lower portion of the rectus abdominis muscle. 2 / 10 Which artery anastomoses with the superior epigastric artery to supply the anterior abdominal wall? A) Inferior epigastric artery B) Obturator artery C) Pubic branch D) Deep circumflex iliac artery The inferior epigastric artery anastomoses with the superior epigastric artery to supply the anterior abdominal wall. 3 / 10 Which artery supplies the lower portion of the rectus abdominis muscle? A) Inferior epigastric artery B) Deep circumflex iliac artery C) Pubic branch D) Umbilical artery The inferior epigastric artery supplies the lower portion of the rectus abdominis muscle. 4 / 10 Which branch of the inferior epigastric artery is unique to females and supplies the round ligament of the uterus? A) Umbilical artery B) Artery of the round ligament C) Deep circumflex iliac artery D) Pubic branch The artery of the round ligament is a branch of the inferior epigastric artery and supplies the round ligament of the uterus. 5 / 10 Which artery continues as the femoral artery after passing under the inguinal ligament? A) Common iliac artery B) Inferior epigastric artery C) External iliac artery D) Internal iliac artery The external iliac artery becomes the femoral artery after passing beneath the inguinal ligament. 6 / 10 Which branch of the external iliac artery anastomoses with the superior epigastric artery? A) Inferior epigastric artery B) Umbilical artery C) Obturator artery D) Deep circumflex iliac artery The inferior epigastric artery, a branch of the external iliac artery, anastomoses with the superior epigastric artery. 7 / 10 Which branch of the inferior epigastric artery supplies the round ligament of the uterus in females? A) Deep circumflex iliac artery B) Pubic branch C) Umbilical artery D) Artery of the round ligament The artery of the round ligament supplies the round ligament of the uterus in females. 8 / 10 Which artery supplies the iliac crest and lateral abdominal wall? A) Inferior epigastric artery B) Deep circumflex iliac artery C) Obturator artery D) Umbilical artery The deep circumflex iliac artery supplies the iliac crest and lateral abdominal wall. 9 / 10 Which artery supplies the spermatic cord in males? A) Pubic branch B) Cremasteric artery C) Deep circumflex iliac artery D) Obturator artery The cremasteric artery, a branch of the inferior epigastric artery, supplies the spermatic cord in males. 10 / 10 Which branch of the external iliac artery supplies the iliac crest and anastomoses with lumbar arteries? A) Inferior epigastric artery B) Obturator artery C) Superior epigastric artery D) Deep circumflex iliac artery The deep circumflex iliac artery supplies the iliac crest and anastomoses with the lumbar arteries. Your score is The average score is 0% Description This video covers the External Iliac Artery (A. Iliaca Externa), its course, branches, and its clinical significance, particularly in surgical applications. Course of the External Iliac Artery: Originates from the common iliac artery. Passes through the vascular space (Lacuna Vasorum) beneath the inguinal ligament. Continues as the femoral artery (A. Femoris) after passing into the thigh. Side Branches of the External Iliac Artery: 1. Deep Circumflex Iliac Artery (Arteria Circumflexa Iliaca Profunda): Runs along the iliac crest. Supplies muscles of the anterior abdominal wall. 2. Inferior Epigastric Artery (Arteria Epigastrica Inferior): Ascends inside the lateral umbilical fold (Plicae Umbilicalis Lateralis). Supplies the rectus abdominis and overlying skin. Gives off several branches: Pubic Branch: Communicates with the pubic branch of the obturator artery, forming an important anastomotic connection known as Corona Mortis (Crown of Death). This anastomosis is significant in surgery because unexpected bleeding from this vessel can be life-threatening. Cremasteric Artery (Arteria Cremasterica): Supplies the cremaster muscle in males and is an important vascular component of the spermatic cord. Artery of the Round Ligament (Arteria Ligamentum Teres Uteri): Analogous to the cremasteric artery, but in females, it supplies the round ligament of the uterus. Clinical Significance: Corona Mortis: Surgeons must be cautious when performing procedures near the pubic branch, as damage to this anastomosis can lead to severe hemorrhage. Inferior Epigastric Artery: Can be a source of collateral circulation in cases of iliac artery occlusion. Hernia Surgery: The inferior epigastric artery is a key landmark when distinguishing direct from indirect inguinal hernias. Sources Used: Memorix Anatomy (2nd Edition) – Hudák Radovan, Kachlík David, Volný Ondřej. Complete Anatomy by 3D4Medical. Biorender. University Notes and Lectures. Transcript Introduction0:00alright so this video is going to be0:02about the common iliac and the external0:04iliac artery0:05and then the next video will be about0:06the internal iliac artery along with0:08some tips on how to remember it easier0:10so as you know the abdominal aorta will0:13continue downwards to approximate the0:15fourth lumbar vertebrae0:17and then it will divide into what is0:18called the common iliac arteries0:21they will continue to approximate the0:23sacroiliac joint as you see here0:25and then further divide into the0:27external iliac0:28and the internal iliac arteries now0:31let’s make a cross-section0:32and look at them both from this0:33perspective to you know visualize them0:35easierCourse0:36now from here we can finally focus on0:38the external iliacare0:40but first let’s look at some important0:41structures to go through0:43you’re probably already familiar with0:44these ligaments but the inguinal0:46ligament0:47together with the iliopectinal arch the0:49pectinal ligament and the lacunar0:51ligament0:52will form two important canals now what0:55were these two canals called0:58muscular and the vascular space or in1:00latin lacunae1:02and lacunae good job if you remember1:03these ones1:05the external iliac artery will run along1:07the terminal line of the pelvic bone as1:09you see here1:10and then eventually go through the1:12vascular space1:14where it will now become the femoral1:15artery
Abdominal Aorta
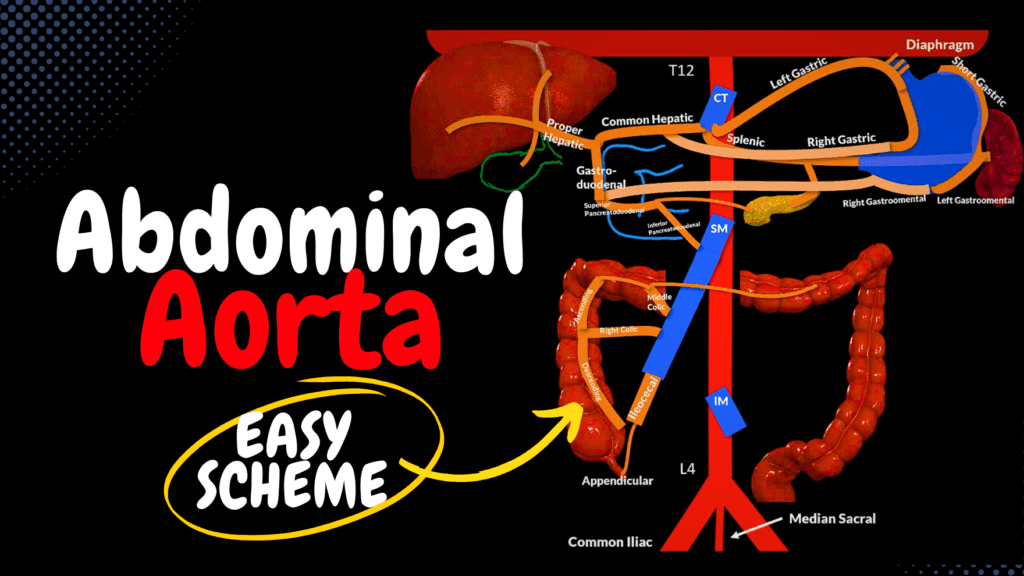
Abdominal Aorta Scheme (Course, Branches, Mnemonics) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript Notes ☆ Member Only Go to PDF Notes Illustrations ☆ Member Only Go to Illustrations 12345678910 Abdominal Aorta – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 Which artery supplies the sigmoid colon? A) Superior rectal artery B) Right colic artery C) Sigmoid arteries D) Left colic artery The sigmoid arteries, branches of the inferior mesenteric artery, supply the sigmoid colon. 2 / 10 Which branch of the inferior mesenteric artery supplies the sigmoid colon? A) Sigmoid arteries B) Right colic artery C) Left colic artery D) Superior rectal artery The sigmoid arteries, branches of the inferior mesenteric artery, supply the sigmoid colon. 3 / 10 Which branch of the superior mesenteric artery supplies the transverse colon? A) Ileocolic artery B) Jejunal arteries C) Right colic artery D) Middle colic artery The middle colic artery, a branch of the superior mesenteric artery, supplies the transverse colon. 4 / 10 Which branch of the celiac trunk supplies the spleen? A) Superior mesenteric artery B) Splenic artery C) Left gastric artery D) Common hepatic artery The splenic artery, a branch of the celiac trunk, supplies the spleen and gives off pancreatic and gastric branches. 5 / 10 Which branch of the celiac trunk supplies the liver? A) Superior mesenteric artery B) Common hepatic artery C) Left gastric artery D) Splenic artery The common hepatic artery, a branch of the celiac trunk, supplies the liver via the proper hepatic artery. 6 / 10 Which artery is the largest branch of the celiac trunk? A) Splenic artery B) Left gastric artery C) Superior mesenteric artery D) Common hepatic artery The splenic artery is the largest branch of the celiac trunk, supplying the spleen and adjacent structures. 7 / 10 Which artery gives rise to the cystic artery? A) Left gastric artery B) Gastroduodenal artery C) Right gastric artery D) Proper hepatic artery The cystic artery, which supplies the gallbladder, arises from the proper hepatic artery. 8 / 10 Which branch of the superior mesenteric artery supplies the appendix? A) Middle colic artery B) Inferior pancreatoduodenal artery C) Appendicular artery D) Right colic artery The appendicular artery, a branch of the ileocolic artery, supplies the appendix. 9 / 10 Which artery forms an anastomosis between the superior and inferior mesenteric arteries? A) Sigmoid arteries B) Marginal artery of Drummond C) Left colic artery D) Right colic artery The marginal artery of Drummond connects the branches of the superior and inferior mesenteric arteries along the colon. 10 / 10 Which artery supplies the diaphragm through the superior suprarenal arteries? A) Middle suprarenal arteries B) Inferior phrenic arteries C) Lumbar arteries D) Renal arteries The inferior phrenic arteries supply the diaphragm and give rise to the superior suprarenal arteries for the adrenal glands. Your score is The average score is 0% Description This video covers the branches of the abdominal aorta, including unpaired visceral branches (supplying digestive organs), paired visceral branches (supplying kidneys, adrenal glands, and gonads), and parietal branches (supplying the diaphragm and abdominal wall). Unpaired Visceral Branches: Celiac Trunk: Left Gastric Artery: Supplies the lesser curvature of the stomach. Splenic Artery: Supplies the spleen and gives off: Pancreatic Branches: Supply the body and tail of the pancreas. Short Gastric Arteries: Supply the fundus of the stomach. Left Gastroomental Artery: Supplies the greater curvature of the stomach. Common Hepatic Artery: Gives off: Right Gastric Artery: Supplies the lesser curvature of the stomach. Proper Hepatic Artery: Supplies the liver and gives rise to: Cystic Artery: Supplies the gallbladder. Gastroduodenal Artery: Supplies the stomach and duodenum, giving off: Right Gastroomental Artery: Supplies the greater curvature of the stomach. Superior Pancreatoduodenal Artery: Supplies the pancreas and duodenum. Superior Mesenteric Artery (Mnemonic: “In My Room I’m Always In Jail”): Ileocolic Artery: Supplies the ileum, cecum, and ascending colon. Appendicular Branch: Supplies the appendix. Inferior Pancreatoduodenal Artery: Supplies the pancreas and duodenum. Middle Colic Artery: Supplies the transverse colon. Right Colic Artery: Supplies the ascending colon. Jejunal and Ileal Branches: Supply the small intestine. Inferior Mesenteric Artery (Mnemonic: “Less”): Left Colic Artery: Supplies the descending colon. Sigmoid Arteries: Supply the sigmoid colon. Superior Rectal Artery: Supplies the rectum. Anastomotic Connection: The Marginal Artery of Drummond connects intestinal arteries, ensuring collateral circulation. Paired Visceral Branches: Middle Suprarenal Arteries: Supply the adrenal glands. Renal Arteries: Supply the kidneys and give off: Inferior Suprarenal Artery: Supplies the adrenal glands. Ureteral Branch: Supplies the ureter. Gonadal Arteries: Supply reproductive organs: Ovarian Arteries: Supply the ovaries. Testicular Arteries: Supply the testes. Parietal Branches: Inferior Phrenic Arteries: Supply the diaphragm. Superior Suprarenal Arteries: Supply the adrenal glands. Lumbar Branches: Supply the posterior abdominal wall. Clinical Correlations: Mesenteric Ischemia: Occlusion of mesenteric arteries can lead to bowel infarction. Abdominal Aortic Aneurysm (AAA): Common in the area of the renal arteries. Nutcracker Syndrome: Compression of the left renal vein between the SMA and aorta. Sources Used: Memorix Anatomy (2nd Edition) – Hudák Radovan, Kachlík David, Volný Ondřej. Complete Anatomy by 3D4Medical. Biorender. University Notes and Lectures. Transcript Introduction0:00all right so this video will be about0:01the abdominal aorta so in the last video0:04we’ll look at the side branches with the0:06thoracic aorta so now let’s move under0:09the diaphragm to look at the abdominal0:11aorta so the abdominal aorta extends all0:14the way from the lower border of the 120:16thoracic vertebrae t12 to the fourth0:19lumbar vertebrae l4 and then it divides0:22into the right and the left common iliac0:24arteries occasionally you may find it0:27continuing between them as the median0:30sacral artery supplying the coccygeal0:32and the pitiful muscle so the abdominalSide Branches0:35aorta has two groups of side branches0:37visceral and parietal branches the0:40visceral supplying the visceral organs0:42and the pirate all supplying everything0:45that’s not the visceral organs so let’s0:47break this down by starting with the0:49visceral branches they are divided into0:52paired and unpaired branches the0:54unpaired visceral branches of the0:57abdominal
Arteries of the Thorax
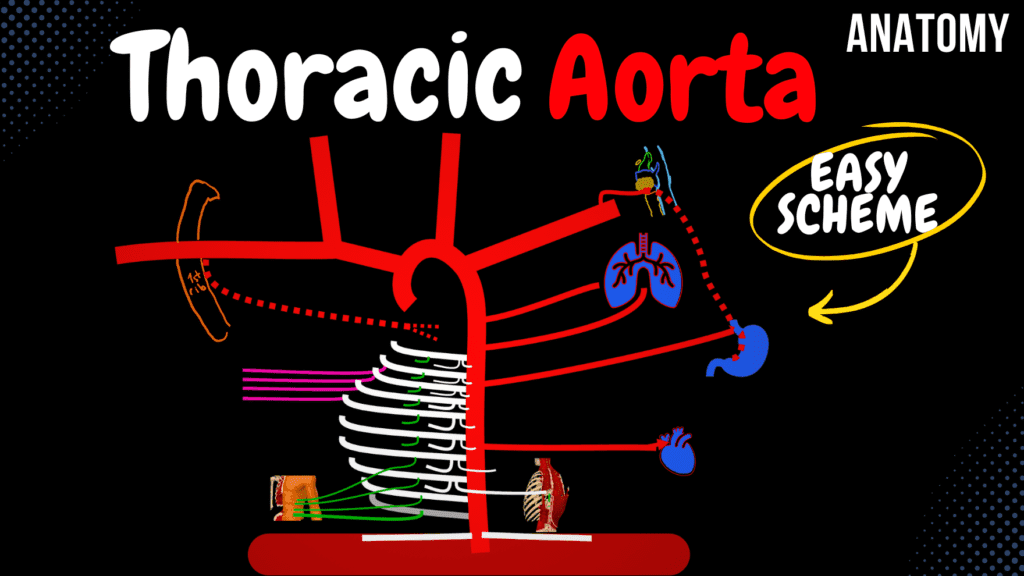
Arteries of the Thorax (Thoracic Aorta) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript Notes ☆ Member Only Go to PDF Notes Illustrations ☆ Member Only Go to Illustrations 12345678910 Thoracic Aorta – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 At which vertebral level does the thoracic aorta begin? A) T3 B) T5 C) T2 D) T4 The thoracic aorta begins at the level of T4, descending along the left side of the vertebral column. 2 / 10 Which parietal branch of the thoracic aorta supplies the diaphragm? A) Mediastinal arteries B) Subcostal arteries C) Superior phrenic arteries D) Posterior intercostal arteries The superior phrenic arteries, arising from the thoracic aorta, supply the superior surface of the diaphragm. 3 / 10 Which branch of the thoracic aorta supplies the lymph nodes of the posterior mediastinum? A) Subcostal arteries B) Mediastinal arteries C) Superior phrenic arteries D) Esophageal arteries The mediastinal arteries, small branches of the thoracic aorta, supply lymph nodes and connective tissue in the posterior mediastinum. 4 / 10 Which visceral branch of the thoracic aorta supplies the lungs, excluding the respiratory part? A) Esophageal arteries B) Bronchial arteries C) Pericardial arteries D) Mediastinal arteries The bronchial arteries supply the lungs, including the bronchi and connective tissue, but not the respiratory portion. 5 / 10 Which branch of the thoracic aorta forms anastomoses with the internal thoracic artery’s branches? A) Subcostal arteries B) Posterior intercostal arteries C) Superior phrenic arteries D) Mediastinal arteries The posterior intercostal arteries form anastomoses with the anterior intercostal arteries from the internal thoracic artery. 6 / 10 Which visceral branches of the thoracic aorta supply the esophagus? A) Mediastinal arteries B) Esophageal arteries C) Bronchial arteries D) Pericardial arteries The esophageal arteries supply the esophagus and form anastomoses with arteries from the neck and abdomen. 7 / 10 Which branch of the thoracic aorta contributes to the blood supply of the posterior mediastinum? A) Posterior intercostal arteries B) Mediastinal arteries C) Subcostal arteries D) Pericardial arteries The mediastinal arteries, small branches of the thoracic aorta, supply the connective tissue and lymph nodes of the posterior mediastinum. 8 / 10 Which branch of the thoracic aorta forms anastomoses with the musculophrenic artery? A) Upper six posterior intercostal arteries B) Subcostal artery C) Lower six posterior intercostal arteries D) Superior phrenic arteries The lower six posterior intercostal arteries form anastomoses with branches of the musculophrenic artery. 9 / 10 Which branch of the thoracic aorta supplies lymph nodes in the posterior mediastinum? A) Pericardial arteries B) Esophageal arteries C) Bronchial arteries D) Mediastinal arteries The mediastinal arteries supply lymph nodes and connective tissues in the posterior mediastinum. 10 / 10 At which vertebral level does the thoracic aorta transition into the abdominal aorta? A) T10 B) T11 C) T12 D) L1 The thoracic aorta transitions to the abdominal aorta at T12, passing through the aortic hiatus of the diaphragm. Your score is The average score is 0% Description This video covers the side branches of the Thoracic Aorta, including both parietal branches (supplying the thoracic wall and diaphragm) and visceral branches (supplying the lungs, esophagus, mediastinum, and pericardium). Parietal Branches: Posterior Intercostal Arteries (3rd–12th rib) The first two intercostal arteries come from the supreme intercostal artery (branch of the costocervical trunk). Upper six posterior intercostal arteries anastomose with the anterior intercostal arteries from the internal thoracic artery. Lower six posterior intercostal arteries anastomose with the anterior intercostal arteries from the musculophrenic branch. Branches of posterior intercostal arteries: Collateral branch: Runs along the lower border of the intercostal space. Lateral cutaneous branch: Supplies the skin and lateral thorax. Dorsal branch: Supplies deep muscles of the back and spinal cord. Lateral mammary artery: Contributes to the blood supply of the breast. Superior Phrenic Artery: Supplies the superior part of the diaphragm. Visceral Branches: Bronchial Artery: Supplies the bronchi, lung parenchyma, and pleura. Mediastinal Artery: Supplies lymph nodes and connective tissue in the posterior mediastinum. Esophageal Artery: Supplies the esophagus along its thoracic portion. Pericardial Artery: Supplies the pericardium surrounding the heart. Clinical Correlations: Coarctation of the Aorta: The posterior intercostal arteries act as collateral circulation in cases of aortic narrowing. Aortic Dissection: The thoracic aorta’s side branches can be affected by aortic wall tears. Esophageal Varices: Enlargement of esophageal veins due to portal hypertension can affect the esophageal artery. Sources Used: Memorix Anatomy (2nd Edition) – Hudák Radovan, Kachlík David, Volný Ondřej. Complete Anatomy by 3D4Medical. Biorender. University Notes and Lectures. Transcript Introduction0:00alright so in this video we’re gonna0:01look at the branches of the thoracic0:03Ulta so by using this picture as a base0:06I think we’ll be able to cover most of0:08the branches supplying the structures of0:10the thoracic cavity one of the most0:13important things you need to know is0:15that the outer starts at the heart going0:17out from the left ventricle as the optic0:20bulb from where the coronary arteries0:22leave and then ascends and then curves0:25forming the optic arch and from the0:27Arctic arch you’re gonna see three major0:30arteries going out the left subclavian0:32artery the left common carotid artery0:35and the breathless a phallic trunk which0:37divides into the right common carotid0:39artery and the right subclavian artery0:42which becomes the axillary artery once0:44it passes the first rib and now after0:47the optic arch it becomes the thoracic0:49aorta which pierces the diaphragm0:52through a hole called the outer Kyoto’s0:55becoming the abdominal aorta so the0:57diaphragm is really the landmark here0:59between the thoracic aorta and the1:01abdominal aorta so the thoracic auto1:05will curve right starts off on the left1:08side of the vertebrae and then ends up1:10in the median line in front of the1:12vertebrae1:13now let’s look into the side branchesSide Branches of the Thoracic Aorta1:14the side branches of the thoracic auto1:17are divided into the visceral and the1:19parallel branches the visceral branches1:22goes to the visceral organs and the1:24parallel branches goes to basically1:27everything that’s not the visceral1:28organs so now let’s first start with theParietal Branches1:31pirate all
Arteries of the Upper Limb
Arteries of the Upper Limb Scheme (Course, Branches, Parts) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript Notes ☆ Member Only Go to PDF Notes Illustrations ☆ Member Only Go to Illustrations 12345678910 Upper Limb Arteries – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 At which anatomical landmark does the brachial artery bifurcate into its terminal branches? A) Elbow B) Axilla C) Wrist D) Cubital fossa The brachial artery bifurcates into the radial and ulnar arteries at the cubital fossa. 2 / 10 Which artery supplies the medial forearm and hand? A) Ulnar artery B) Radial artery C) Brachial artery D) Axillary artery The ulnar artery supplies the medial forearm, hand, and contributes to the superficial and deep palmar arches. 3 / 10 Which branch of the radial artery contributes to the deep palmar arch? A) Ulnar artery B) Radial artery C) Anterior interosseous artery D) Posterior interosseous artery The deep palmar arch is primarily formed by the radial artery, which contributes significantly to its structure. 4 / 10 Which branch of the ulnar artery participates in the deep palmar arch? A) Superficial palmar arch B) Radial artery C) Anterior interosseous artery D) Deep palmar branch The deep palmar branch of the ulnar artery contributes to the deep palmar arch in the hand. 5 / 10 Which artery gives rise to the anterior and posterior interosseous arteries? A) Radial artery B) Ulnar artery C) Brachial artery D) Superficial palmar arch The ulnar artery gives rise to the common interosseous artery, which divides into the anterior and posterior interosseous arteries. 6 / 10 Which branch of the axillary artery supplies the latissimus dorsi muscle? A) Superior thoracic artery B) Lateral thoracic artery C) Thoracodorsal artery D) Thoracoacromial artery The thoracodorsal artery, a branch of the subscapular artery, supplies the latissimus dorsi muscle. 7 / 10 Which artery passes through the anatomical snuffbox? A) Ulnar artery B) Brachial artery C) Superficial palmar arch D) Radial artery The radial artery passes through the anatomical snuffbox on the dorsum of the hand. 8 / 10 Which artery supplies the deep structures of the posterior forearm? A) Ulnar artery B) Radial artery C) Posterior interosseous artery D) Anterior interosseous artery The posterior interosseous artery, a branch of the common interosseous artery, supplies the posterior compartment of the forearm. 9 / 10 Which branch of the brachial artery supplies the posterior compartment of the arm? A) Superior ulnar collateral B) Profunda brachii artery C) Radial artery D) Ulnar artery The profunda brachii artery, a branch of the brachial artery, supplies the posterior compartment of the arm, including the triceps brachii. 10 / 10 Which artery supplies the lateral side of the palm and the thumb? A) Radial artery B) Ulnar artery C) Superficial palmar arch D) Deep palmar arch The radial artery supplies the lateral side of the palm and the thumb through its branches, including the princeps pollicis artery. Your score is The average score is 0% Description This video will cover: Branches of the Axillary Artery Branches of the Brachial Artery Blood supply of the Elbow (Rete Cubiti) Branches of the Radial Artery Branches of the Ulnar Artery Blood supply of the Wrist (Rete Carpale) Blood supply of the Hand Axillary Artery: Divided into three parts based on its relation to the pectoralis minor muscle: 1st part (medial to pectoralis minor): Superior Thoracic Artery 2nd part (behind pectoralis minor): Thoracoacromial Artery (Mnemonic: APCD) A: Acromial Branch P: Pectoral Branch C: Clavicular Branch D: Deltoid Branch Lateral Thoracic Artery Lateral Mammary Artery 3rd part (lateral to pectoralis minor): Subscapular Artery Thoracodorsal Artery Circumflex Scapular Artery Anterior Circumflex Humeral Artery Posterior Circumflex Humeral Artery Brachial Artery: Located in the medial bicipital groove, supplying the arm. Branches supplying anterior arm muscles Deep Brachial Artery Medial Collateral Artery Radial Collateral Artery Inferior Ulnar Collateral Artery Superior Ulnar Collateral Artery Ulnar Artery: Recurrent Ulnar Arteries Common Interosseous Artery Anterior Interosseous Artery Posterior Interosseous Artery Recurrent Interosseous Artery Radial Artery: Superficial Palmar Artery Palmar Carpal Artery Dorsal Carpal Artery Principal Artery of the Thumb Blood Supply of the Elbow (Rete Cubiti): Radial Collateral Artery ↔ Recurrent Radial Artery Medial Collateral Artery ↔ Recurrent Interosseous Artery Superior Ulnar Collateral Artery ↔ Posterior Branch of Recurrent Ulnar Artery Inferior Ulnar Collateral Artery ↔ Anterior Branch of Recurrent Ulnar Artery Blood Supply of the Wrist (Rete Carpale): Anterior Carpal Plexus (Rete Carpi Palmare) Palmar Carpal Arch/Plexus Posterior Carpal Plexus (Rete Carpi Dorsale) Dorsal Carpal Arch/Plexus Posterior Interosseous Artery Anterior Interosseous Artery Blood Supply of the Hand: Palm of the Hand: Superficial Palmar Arch Common Palmar Digital Arteries Proper Palmar Digital Arteries Deep Palmar Arch Princeps Pollicis Artery Palmar Digital Arteries Palmar Metacarpal Arteries Dorsum of the Hand: Dorsal Carpal Network Dorsal Metacarpal Arteries Dorsal Digital Arteries Sources Used: Memorix Anatomy (2nd Edition) – Hudák Radovan, Kachlík David, Volný Ondřej. Complete Anatomy by 3D4Medical. Biorender. University Notes and Lectures. Transcript Introduction0:00our so this video is about the arterial0:02blood supply of the upper limb all the0:05way from the axillary artery until the0:07tip of your fingers so as you know the0:10outer leaves the heart giving off the0:12left common carotid artery the left0:15subclavian and the Braja cephalic trunk0:17which divides into the right common0:19carotid artery and the right subclavian0:21now from here we’re gonna have to follow0:24the subclavian artery as the major blood0:27supply to the upper extremities comes0:29from the subclavian artery now as soon0:32as the subclavian artery passes the0:35first rib is going to become the0:37axillary artery and this is really where0:40we’re going to start the axillary artery0:43is going to pass through the axilla and0:45then when it reaches the lower border of0:47the teres module it will continue as the0:50brachial artery now this landmark really0:53depends from textbook to textbook in0:55some places you could see it written as0:57the free margin of the pectoralis minor0:59would that reminds the border between1:01the axillary and the brachial artery
