Hypersensitivity Reactions
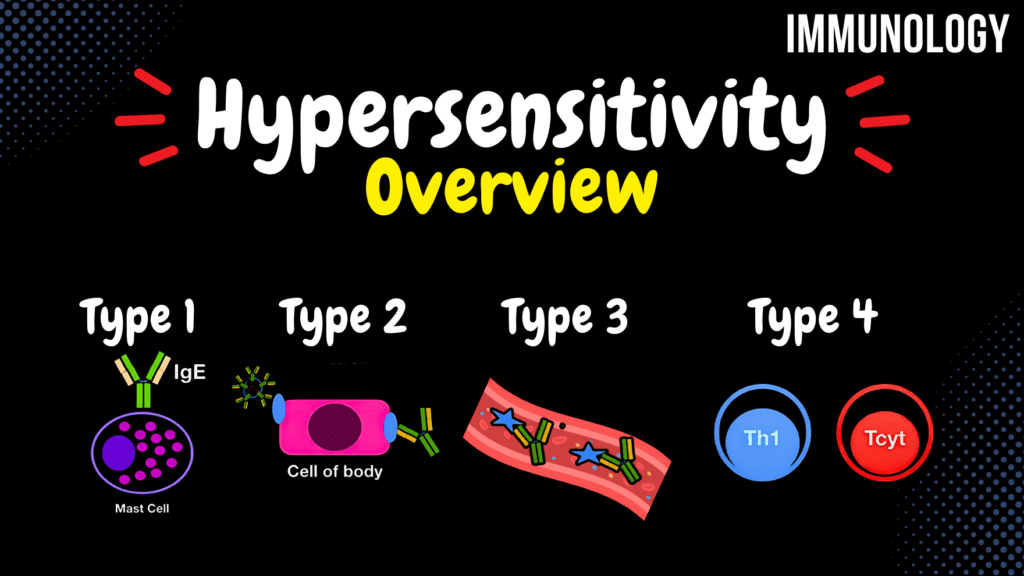
Hypersensitivity Reactions (Type 1-4) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript 📢 Currently, there is no PDF for this video.If you’re interested in having one, feel free to send an inquiry, and I may create it in the future. BUT! There’s a quiz available in the next tab. 12345678910 Hypersensitivity – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 What is the mechanism of action of granulysin in Type 4 hypersensitivity? A) Neutralizes cytokines B) Enhances inflammation C) Activates complement D) Induces apoptosis Granulysin induces apoptosis of target cells during Type 4 hypersensitivity. 2 / 10 Which hypersensitivity type involves immune responses against viral budding antigens? A) Type 4 B) Type 3 C) Type 1 D) Type 2 Type 2 hypersensitivity occurs when antibodies target antigens during viral budding. 3 / 10 Which hypersensitivity reaction is most commonly associated with poison ivy exposure? A) Type 2 B) Type 4 C) Type 3 D) Type 1 Poison ivy causes a Type 4 hypersensitivity reaction. 4 / 10 Which cells are directly affected in Type 2 hypersensitivity? A) Epithelial cells B) Target cells C) Neutrophils D) T-cells Target cells, such as red blood cells, are destroyed by antibodies and complement in Type 2 hypersensitivity. 5 / 10 What is the function of histamine in Type 1 hypersensitivity? A) Increases vascular permeability B) Neutralizes cytokines C) Activates T-cells D) Opsonizes antigens Histamine causes vasodilation, increased vascular permeability, and bronchoconstriction. 6 / 10 What is the clinical hallmark of Type 3 hypersensitivity? A) Histamine release B) Mast cell activation C) Immune complex deposition D) Cytokine storm Immune complex deposition in tissues is the hallmark of Type 3 hypersensitivity. 7 / 10 What is the primary cell type involved in Type 1 hypersensitivity? A) T-lymphocytes B) Neutrophils C) Macrophages D) Mast cells Mast cells are key players in Type 1 hypersensitivity as they release histamine upon activation. 8 / 10 What is a key feature of Type 4 hypersensitivity? A) Delayed response B) Immediate response C) Antibody involvement D) Complement activation It is delayed, as T-cell responses take 24-72 hours to cause inflammation. 9 / 10 Which type of hypersensitivity involves antibody-dependent cell-mediated cytotoxicity? A) Type 4 B) Type 2 C) Type 3 D) Type 1 Type 2 hypersensitivity involves antibody-dependent cytotoxicity via natural killer cells. 10 / 10 What are the key effector cells in Type 3 hypersensitivity? A) Basophils B) Mast cells C) Neutrophils D) T-lymphocytes Neutrophils are key effector cells that cause tissue damage in Type 3 hypersensitivity. Your score is The average score is 0% Description This video is about Hypersensitivity and its classification. All information in my immunology videos is sourced from: Book: Immunology, Eighth Edition by David Male, Jonathan Brostoff, David Roth, and Ivan Roitt Additional research: PubMed University lecture materials Hypersensitivity: Excessive Immune Response Hypersensitivity reactions occur when the immune system responds excessively to an antigen, leading to tissue damage. Coombs and Gell Classification of Hypersensitivity: Type 1: Immediate Hypersensitivity (IgE-mediated) Type 2: Antibody-Mediated Hypersensitivity Type 3: Immune Complex Disease Type 4: Cell-Mediated Reactions Type 1 Hypersensitivity: IgE-Mediated Hypersensitivity Occurs when IgE antibodies on mast cells trigger anaphylactic shock. Factors that Induce Allergy: Pollen Inhaled particles (dust, pet dander, mold spores) Milk, fish, nuts Direct skin contact allergens Genetic predisposition plays a role in allergic hypersensitivity. Development of Type 1 Hypersensitivity: First exposure: Inhaled pollen enters the body. Phagocytosis: Langerhans cells (or other APCs) phagocytose pollen and travel to the lymph node via afferent lymphatic vessels. Sensitization Stage (in the lymph node): APCs present the antigen on MHCII to a naive T-helper cell. Three activation signals occur: TCR-MHCII, CD28-B7, and IL-4. IL-2 promotes Th0 proliferation into effector Th2 cells. B-cells that bind pollen undergo receptor-mediated endocytosis and interact with Th2, leading to IgE production. Sensitization phase duration: 6 months to 5 years. Second exposure: Pollen binds to IgE antibodies on mast cells. Mast cell degranulation: Histamine is released, leading to: Vasodilation Increased capillary permeability Bronchoconstriction Secretion of IL-5 and TNF-α Type 2 Hypersensitivity: Antibody-Mediated Immune Response Involves IgG or IgM antibodies targeting cell surface antigens. Possible Causes: Viral Budding: Some viruses place their proteins on the host cell surface, leading to antibody recognition. Blood Transfusion Reactions: Mismatched ABO blood types can trigger immune destruction of red blood cells. Drug Allergies: Some drugs can bind to cell surfaces, making them targets for antibodies. Autoimmune Reactions: T-cell tolerance failure can lead to autoimmune diseases. Mechanism: Antibodies bind to surface antigens. Activation of the Complement System: MAC formation leads to cell lysis. C3b opsonization allows phagocytes to bind via C3b receptors. Neutrophils and NK cells recognize and destroy the antibody-coated cells. Type 3 Hypersensitivity: Immune Complex Disease Immune complexes (antigen-antibody complexes) form and deposit in tissues, causing inflammation. Pathophysiology: Normally, immune complexes are cleared by the liver and spleen. If they persist, they can become trapped in vessel walls, activating the complement system. Neutrophils, basophils, and mast cells respond, leading to inflammation (Arthus Reaction). Platelets aggregate, further worsening the reaction. Examples: Serum Sickness: If bitten by a venomous snake, injecting anti-venom (pre-formed antibodies) can cause immune complex formation. Systemic Lupus Erythematosus (SLE): Persistent immune complexes cause chronic inflammation. Type 4 Hypersensitivity: Cell-Mediated (Delayed-Type Hypersensitivity) Involves Th1 and T-cytotoxic (T-cyt) cells triggering local inflammation. Example: Tuberculin Skin Test (Mantoux Test) Injection: Tuberculin is injected into the skin. Phagocytosis: Macrophages or Langerhans cells engulf tuberculin. Antigen Presentation: APCs travel to the lymph node and present tuberculin on: MHCII to naive Th0 cells. MHCI to naive T-cytotoxic cells. Th1 Activation: Three activation signals occur. IL-2 helps differentiation into effector Th1. T-cyt Activation: IL-2 and IFN-γ promote differentiation into effector T-cytotoxic cells. Effector T-cyt expresses FasL, which binds Fas on infected cells. Releases perforins and granzymes, causing apoptosis. Second exposure: Phagocytes activate effector Th1 and T-cytotoxic cells. Th1 releases IFN-γ to activate macrophages. Macrophages release inflammatory cytokines
Cellular Immunity
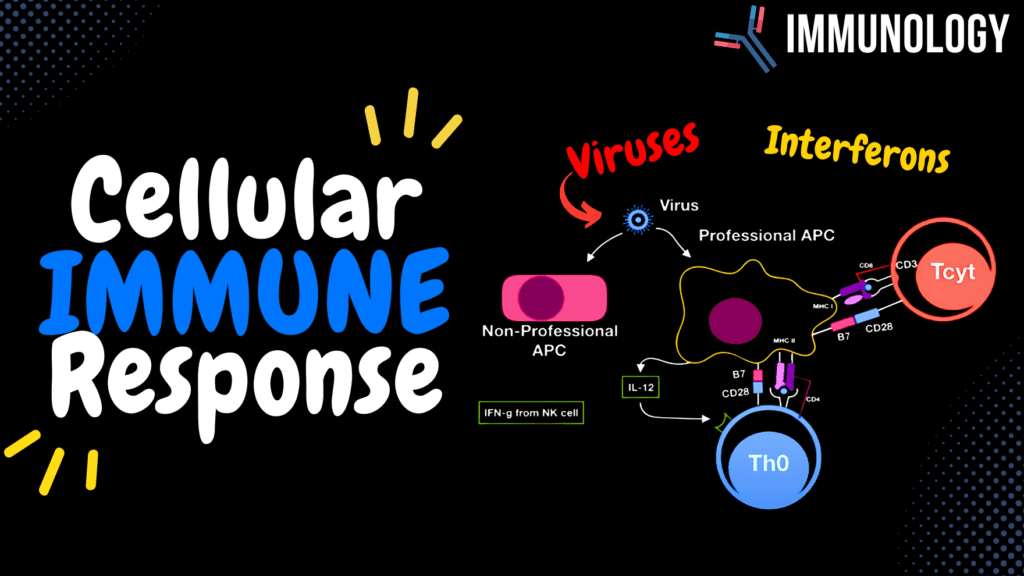
Cellular Immunity (T-Cytotoxic, NK Cell, Macrophage, Immunity To Virus, Interferons) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript 📢 Currently, there is no PDF for this video.If you’re interested in having one, feel free to send an inquiry, and I may create it in the future. BUT! There’s a quiz available in the next tab. 12345678910 Cellular Immune Response – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 What is the role of CD28 on T-cytotoxic cells? A) Activates NK cells B) Enhances cytokine release C) Suppresses inflammation D) Provides co-stimulation CD28 binds B7 on APCs to provide a co-stimulatory signal for T-cell activation. 2 / 10 What is the role of IL-12 in cellular immunity? A) Neutralizes cytokines B) Suppresses Th2 response C) Activates B cells D) Promotes Th1 differentiation IL-12 is released by macrophages to promote Th1 differentiation and NK cell activation. 3 / 10 What is the primary function of Type I interferons (IFN-alpha and IFN-beta)? A) Activate Th2 cells B) Inhibit viral replication C) Reduce inflammation D) Neutralize antibodies Type I interferons inhibit viral replication and increase MHCI expression. 4 / 10 What cytokine promotes Th1 differentiation and inhibits Th2 function? A) IL-2 B) TNF-alpha C) IL-4 D) IFN-gamma IFN-gamma promotes Th1 differentiation and reduces Th2 response. 5 / 10 Which innate immune cells release cytokines to initiate a cellular immune response? A) B-cells B) Macrophages C) NK cells D) Dendritic cells Macrophages release IL-12 and other cytokines to initiate cellular immunity. 6 / 10 What triggers natural killer cells to kill a target cell? A) Activation of Th2 cells B) Absence of MHCI C) Presence of CD4 D) High MHCI expression NK cells kill cells lacking MHCI or expressing stress signals. 7 / 10 What is the role of FasL on T-cytotoxic cells? A) Inhibits T-cell growth B) Promotes Th1 differentiation C) Binds to cytokines D) Induces apoptosis FasL binds to Fas on infected cells, inducing apoptosis. 8 / 10 Which receptor on NK cells inhibits killing when bound to MHCI? A) NKR-P1 B) Ly49 C) CD16 D) FasL Ly49 receptor binds MHCI and sends an inhibitory signal to NK cells. 9 / 10 What cytokine is involved in recruiting neutrophils during a cellular immune response? A) TNF-alpha B) IL-4 C) IL-12 D) IL-8 IL-8 recruits neutrophils during cellular immunity. 10 / 10 What is the outcome of decreased MHCI expression on virus-infected cells? A) Promotes antibody production B) Enhances inflammation C) Triggers NK cell cytotoxicity D) Activates Th2 cells Decreased MHCI triggers NK cells to kill the infected cells. Your score is The average score is 0% Description PS! At 02:00, I incorrectly wrote MHCII instead of MHCI in the list of activation signals. I apologize for the typo, viewers! This video covers the Cellular Immune Response, its effectors, and mechanisms of immunity against viruses. All information in my immunology videos is sourced from: Book: Immunology, Eighth Edition by David Male, Jonathan Brostoff, David Roth, and Ivan Roitt Additional research: PubMed University lecture materials Types of Immune Responses: Humoral Immune Response Cellular Immune Response Immunological Memory/T-cell Tolerance Hypersensitivity Cellular Immune Response Targets: Virus-infected cells Oncogenic cells (Cancer cells) Transplanted cells These are controlled through MHCI on their surface. Effector Cells in Cellular Immunity: T-Cytotoxic Cells Natural Killer (NK) Cells Macrophages T-Cytotoxic Lymphocyte Activation: Requires three activation signals: T-cell receptor (TCR) with CD8 and CD3 binds to MHCI. CD28 – B7 interaction. Cytokines (IFN-γ and IL-2) from Th1. Once activated, T-cytotoxic cells express Fas Ligand (FasL), which binds to Fas on infected cells. They then release perforins and granzymes to induce apoptosis. Natural Killer (NK) Cells: Differentiate between healthy and infected cells based on surface receptors: NK Cell Surface Receptors: Ly49: Binds to MHCI and sends a negative signal to prevent NK activation. NKR-P1: Recognizes proteins on infected cells and activates NK cells. Fas-L: Recognizes Fas-expressing sick cells. CD16: Binds to the Fc portion of antibodies, triggering antibody-dependent cytotoxicity. IL-2 receptor: Binds to IL-2 and activates NK cells. Surface markers: CD56+, CD16+, and CD2 (adhesion molecule). Activated NK Cells Release: TNF-α: Activates endothelium and induces fever. IFN-γ: Enhances cytotoxicity, activates macrophages, and further stimulates NK cells. Scenario of Cytotoxic Immune Response: A virus infects a normal cell, making it a non-professional APC (does not express B7). If a professional APC phagocytoses the infected cell, it presents viral fragments on MHC I and MHC II. T-cytotoxic cell binds to MHC I via TCR-MHCI and CD28-B7. Naïve Th0 binds to MHC II via TCR-MHCII, B7-CD28, and receives IL-12 → releases IL-2 (autocrine) → differentiates into Th1. Effector Th1 releases IFN-γ and IL-2 to fully activate T-cytotoxic cells. Effector T-cytotoxic cells express FasL, bind to Fas on infected cells, and release Granzyme B and Perforins to induce apoptosis. Th1 activates macrophages via CD40L-CD40 and IFN-γ to eliminate remaining viral particles. Immunity to Viruses: Adaptive Immune Response: Involves T-cells, resulting in immunological memory and antibody production. Innate Immune Factors: General Factors: Viruses have specific cell receptors (tropism). Macrophages release inflammatory cytokines, inducing fever. Secretory factors: Feces, saliva, gastric juice. Humoral Factors: Complement System (opsonization). Acute-phase proteins (Mannose Binding Lectin and C-Reactive Protein). Cellular Factors: Phagocytosis Interferons Interferon System: Interferons (IFNs) are cytokines released in response to viral infection. Types of Interferons: IFN-α: Released by leukocytes. IFN-β: Released by fibroblasts. IFN-γ: Released by immune cells. Classification: Type 1 IFN (IFN-α, IFN-β): Inhibits protein synthesis and DNA replication in virus-infected cells. Increases MHCI expression on all cells. Activates NK cells. Stimulates T-helper and B-lymphocytes. Type 2 IFN (IFN-γ): Reduces Th2 response. Enhances Th1 response. Activates NK cells and macrophages. Differentiates B-cells into IgG-secreting plasma cells. Antibodies Against Viruses: 1st week: IgM (Neutralizes circulating viruses). 2nd week: IgG (Targets circulating and extravascular viruses). IgA: Protects mucosal surfaces and prevents reinfection. Summary: When a cell is infected by a virus: It expresses Fas, which binds to
Humoral Immunity
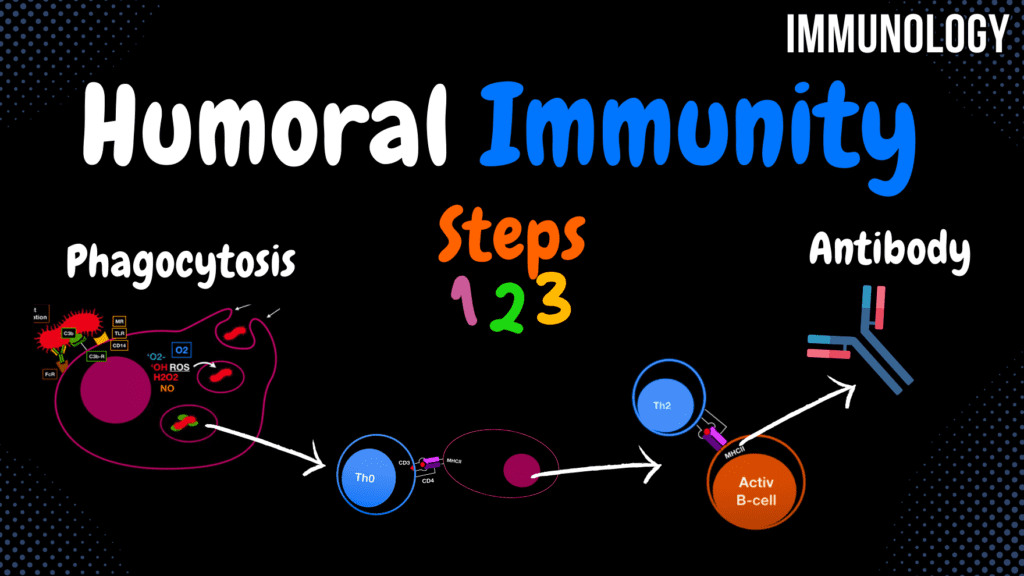
Humoral Immunity (ALL Steps) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript 📢 Currently, there is no PDF for this video.If you’re interested in having one, feel free to send an inquiry, and I may create it in the future. BUT! There’s a quiz available in the next tab. 12345678910 Humoral Immunity – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 What is the role of CRP (C-reactive protein) during inflammation? A) Acts as an opsonin B) Enhances cytokine release C) Inhibits T-cell function D) Stimulates IgE CRP acts as an opsonin and activates the classical complement pathway. 2 / 10 What is the primary purpose of the humoral immune response? A) Direct phagocytosis B) Promote cell apoptosis C) Antibody production D) Inhibit T-cell activation To target extracellular pathogens through antibody production. 3 / 10 What cytokine activates B-cells during T-cell-dependent B-cell differentiation? A) IL-6 B) IL-4 C) TNF-alpha D) IL-12 IL-4 is essential for activating B-cells during T-cell-dependent B-cell differentiation. 4 / 10 What is the primary role of the humoral immune response? A) Phagocytose pathogens B) Kill infected cells C) Produce antibodies D) Release cytokines The humoral immune response involves producing antibodies to target extracellular pathogens. 5 / 10 What is the primary role of IL-6 during the humoral immune response? A) Induces apoptosis B) Suppresses Th1 response C) Activates B- and T-cells D) Inhibits inflammation IL-6 promotes the activation of B- and T-lymphocytes. 6 / 10 What triggers T-independent B-cell activation? A) CD40-CD40L B) IL-4 C) Direct carbohydrate binding D) IL-12 T-independent activation occurs when carbohydrates bind directly to the B-cell receptor. 7 / 10 What happens to the level of IgM during the secondary immune response? A) Decreases significantly B) Remains constant C) Increases drastically D) Stops production The level of IgM remains the same during the secondary immune response. 8 / 10 Which receptor on phagocytes binds to the Fc region of antibodies for direct opsonization? A) TLR B) CD14 C) C3b receptor D) Fc receptor The Fc receptor binds to the Fc region of antibodies to promote direct opsonization. 9 / 10 What happens to the level of IgG during a secondary humoral immune response? A) Becomes undetectable B) Remains constant C) Decreases D) Increases IgG levels increase rapidly and are higher than in the primary response. 10 / 10 How do acute-phase proteins like CRP and MBL function in humoral immunity? A) Promote phagocytosis B) Activate NK cells C) Neutralize toxins D) Opsonize and activate They act as opsonins and activate the complement system. Your score is The average score is 0% Description This video covers the humoral immune system and its role in immune responses. All information in my immunology videos is sourced from: Book: Immunology, Eighth Edition by David Male, Jonathan Brostoff, David Roth, and Ivan Roitt Additional research: PubMed University lecture materials Types of Immune Responses: Humoral Immune Response Cellular Immune Response Immunological Memory/T-cell Tolerance Hypersensitivity Steps in Humoral Immunity: Antigen Entry: Extracellular antigens enter the body. Phagocytosis and Inflammation: Professional phagocytes attack the antigen. Antigen Presentation: Peptides presented on MHC II to Th0 cells. B-cell Differentiation: Specific antibodies are produced. Phagocytosis and Inflammation: Professional Phagocytes: Neutrophils Macrophages/Monocytes Mast Cells Dendritic Cells Steps in Phagocytosis: Binding: Mannose Receptor: Binds mannose on microbial surfaces. Toll-Like Receptor (TLR): Recognizes microbial patterns. CD14: Binds lipopolysaccharide (LPS) of Gram-negative bacteria. C3b – C3b Receptor: Indirect opsonization (enhances binding). Fc-Receptor: Binds to the Fc portion of antibodies (direct opsonization). Engulfment: Formation of pseudopods to enclose the antigen. Phagosome Formation: Oxygen-dependent digestion via Reactive Oxygen Species (ROS). Lysosome Fusion: Breakdown of microbes via: Enzymes (Proteolytic, Hydrolytic) Antimicrobial Peptides (Defensins) Acidic Reactions (Low pH) Lactoferrin (Neutrophils) Antigen Presentation: Fragments of the microbe are displayed on MHC II. Pro-Inflammatory Cytokine Release: IL-8: Chemotaxis for leukocytes. IL-1: Activates T-lymphocytes and macrophages. IL-6: Activates T- and B-lymphocytes. TNF-α: Activates endothelium, promoting neutrophil extravasation. IL-12: Activates natural killer (NK) cells. Systemic Response of IL-1, IL-6, and TNF-α: They act as endogenous pyrogens (cause fever). Travel to the hypothalamus → Release Prostaglandin E2 (PGE2) → Increases body temperature. IL-6 travels to the liver → Stimulates release of acute-phase proteins (CRP and MBL). Incomplete Phagocytosis: Some microbes evade destruction inside the phagocyte: Listeria: Releases Listeriolysin. Mycobacterium: Releases Catalase. Activation of Naïve T Helper Cells: Three activation signals are needed: 1st Signal: TCR (with CD4/CD3) binds to MHC II. 2nd Signal: B7 binds to CD28. 3rd Signal: IL-4 (from mast cells/Th1). Naïve Th0 releases IL-2 (autocrine) to promote its growth. Th0 undergoes clonal expansion and differentiates into effector Th2 cells. Effector Th2 Functions: Expresses CD40L to assist B-cell activation. Releases cytokines: IL-10: Suppresses Th1 function. IL-4, IL-5, IL-6: Stimulate B-cell differentiation. B-Cell Activation in Secondary Lymphoid Organs: B-cells have B-cell Receptors (BCR): IgD/IgM with Iga and Igb signaling components. B-cells migrate to the secondary follicle to interact with T-cells. Three Activation Signals for Naïve B-Cell Differentiation (T-cell Dependent): 1st Signal: BCR binds to antigen. 2nd Signal: B-cell binds to active Th2 via: MHC II – TCR CD40 – CD40L 3rd Signal: IL-4, IL-5, IL-6, IL-10, IL-2, IFN-γ (determines antibody class). B-cells then differentiate into: Memory B-cells (long-term immunity). Plasma Cells (produce antibodies). T-Independent B-Cell Differentiation: Occurs when BCR binds to polysaccharides or carbohydrate antigens. Strong activation signal → Differentiation into IgM-secreting Plasma Cells. Does not produce memory B-cells. Primary vs. Secondary Humoral Immune Response: Primary Response: First exposure: IgM is produced first, followed by IgG. IgG levels are higher than IgM. Secondary Response: Second exposure: IgM response is the same. IgG response is stronger and faster due to memory B-cells. Transcript No transcript available for this video. Notes & Illustrations Quizzes Summary & Transcript 📢 Currently, there is no PDF for this video.If you’re interested in having one, feel free to send an inquiry, and I may create it in the future. BUT! There’s a quiz available
T-Cells
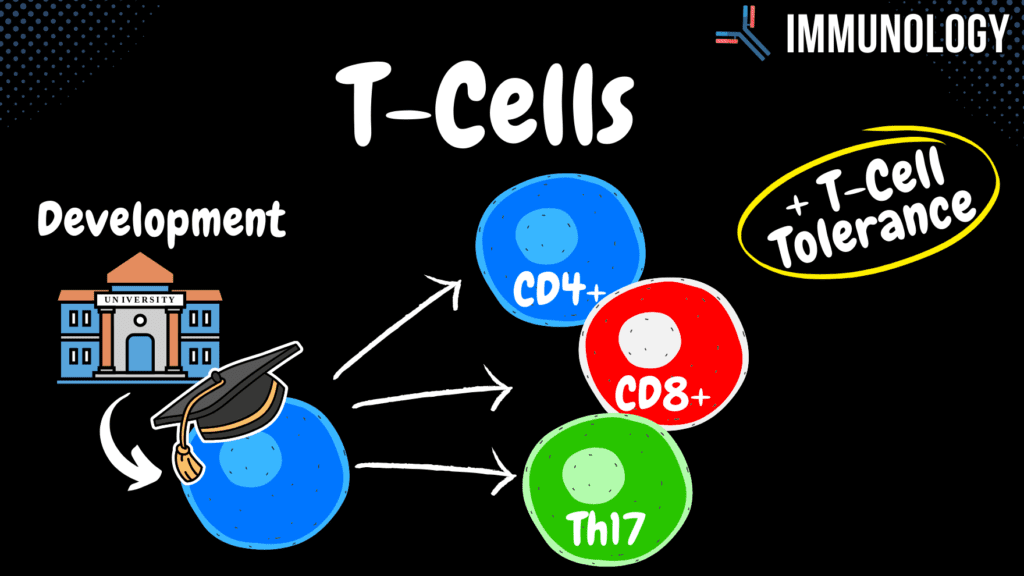
T- Cells (Development, Helper CD4+, Cytotoxic CD8+, Th17, Tolerance) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript 📢 Currently, there is no PDF for this video.If you’re interested in having one, feel free to send an inquiry, and I may create it in the future. BUT! There’s a quiz available in the next tab. 12345678910 T-Cells – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 What organ is responsible for T-cell maturation? A) Lymph nodes B) Bone marrow C) Thymus D) Spleen The thymus is the primary site for T-cell maturation. 2 / 10 What surface molecule mediates macrophage activation by Th1 cells? A) FasL B) MHC I C) CD40L D) IL-2 CD40L on Th1 cells interacts with CD40 on macrophages to activate them. 3 / 10 What is the primary function of T-regulatory cells? A) Activate macrophages B) Promote Th1 function C) Suppress immune response D) Stimulate antibody production T-regulatory cells suppress the immune response and prevent autoimmunity. 4 / 10 What is the purpose of positive selection in T-cell development? A) Prevent apoptosis B) Recognize self MHC C) Induce clonal expansion D) Check for antigen recognition Positive selection ensures that T-cells can recognize self MHC molecules. 5 / 10 Which molecule is involved in the first activation signal for naive T-cells? A) MHC-TCR B) CD40-CD40L C) FasL-Fas D) B7-CD28 The interaction between MHC and TCR (with CD4 or CD8) constitutes the first activation signal. 6 / 10 What is the role of IL-10 released by T-regulatory cells? A) Recruit neutrophils B) Suppress Th1 response C) Stimulate Th2 cells D) Activate dendritic cells IL-10 suppresses Th1 responses and promotes immune tolerance. 7 / 10 What role does IL-2 play in T-cell activation? A) Activates dendritic cells B) Enhances T-cell growth C) Promotes inflammation D) Suppresses Th1 cells IL-2 promotes the clonal expansion of activated T-cells. 8 / 10 Which T-cell subset is most effective against viral infections? A) Cytotoxic T-cells B) T-regulatory cells C) Th1 cells D) Th17 cells CD8+ T-cells (cytotoxic T-cells) are highly effective against viral infections. 9 / 10 What happens during clonal expansion of T-cells? A) Present antigens B) Proliferate C) Suppress inflammation D) Undergo apoptosis Activated T-cells proliferate and differentiate during clonal expansion. 10 / 10 How do T-cells recognize antigens? A) CD40-CD40L B) TCR on MHC C) TGF-beta D) BCR on MHC T-cells recognize antigens via the T-cell receptor (TCR) presented on MHC molecules. Your score is The average score is 0% Description This video is about T-Lymphocyte Development and Function. All information in my immunology videos is sourced from: Book: Immunology, Eighth Edition by David Male, Jonathan Brostoff, David Roth, and Ivan Roitt Additional research: PubMed University lecture materials Development of T-Lymphocytes: Origin: In red bone marrow as Multipotent Lymphoid Stem Cells. Migration: Travel to the Thymus for further development. Thymus: Grows to its maximum size around puberty, then gradually replaced by fat tissue. Stages of T-cell Development in the Thymus: Double Negative Stage: Ensure the cell lacks CD4/CD8. Double Positive Stage: Ensure the cell expresses CD4/CD8. Positive Selection: Ensure recognition of self MHC. Negative Selection: Ensure no recognition of self-antigens. Single Positive Selection: Cells become either: CD4+ T-Helper Cells CD8+ Cytotoxic T-Cells Survivors travel to secondary lymphoid organs. If a cell fails any stage, it undergoes apoptosis. CD4+ Activation – T Helper Cells: Requires 3 activation signals to activate naïve T-cells: 1st Activation Signal: MHC – TCR (Receptor + CD4 + CD3). 2nd Activation Signal: B7 – CD28. 3rd Activation Signal: Cytokines: IL-4: Induces differentiation into Th2. IL-12: Induces differentiation into Th1. Activated T-helper cells secrete IL-2 (autocrine) for self-proliferation. Functions of Activated T-Helper Cells: Th2 Cells: IL-10: Suppresses Th1 response. IL-4, IL-5, IL-6: Stimulate B-cells for IgG, IgE, and IgA synthesis. Th1 Cells (Inflammatory T-Helper Cells): IFN-γ (Interferon Gamma): Activates macrophages, promotes IgG synthesis, and inhibits Th2 response. IL-2: Helps the growth of B-cells and T-cells. CD8+ Activation – Cytotoxic T-Cells: Virus-infected cells present antigen on: MHC I: Non-professional APCs. MHC II and MHC I: Professional APCs. Activation: T-Cytotoxic Cell binds to MHC I through TCR (3 activation signals required). Th0 binds to MHC II and differentiates into Th1, releasing: IFN-γ and IL-2 to enhance cytotoxic T-cell activity. Mechanism of Killing: T-cytotoxic cells undergo clonal expansion and express Fas-L to target Fas-expressing infected cells. Release of: Perforin: Creates holes in the infected cell membrane. Granzyme B: Induces DNA fragmentation. Th17 Cells: Important in fighting fungal infections. Severe fungal infections occur in immunosuppressed individuals. Th17 Cell Development: Macrophages phagocytose fungi. Present three activation signals to naïve T-helper cells (Th0). Macrophages release: IL-1, IL-6, IL-23 Transforming Growth Factor Beta (TGF-β) → This differentiates Th0 into Th17. Th17 Cell Functions: IL-17: Recruits neutrophils. Neutrophils: Promote inflammation via: Granule release Lysozymes Reactive oxygen species IL-22 and IL-17: Stimulate epithelial cells to produce antimicrobial defensins. T-Cell Tolerance: Eliminates cells that react to self-antigens. Central Tolerance (In Thymus): Kills self-reactive T-cells before they mature. Peripheral Tolerance (Outside Thymus): Self-reactive T-cells that escape to secondary lymphoid organs are inhibited through: Clonal deletion (Direct inactivation). T-Regulatory Cells (T-reg). T-Regulatory Cell (T-Reg) Functions: IL-35: Suppresses immune function. IL-10: Decreases Th1 function. TGF-β: Inhibits macrophages. Regulates dendritic cells to prevent excessive immune response. Monitors IL-2 levels to regulate immune function. How Many Days Does It Take to Gain Immunological Memory? Starts as a naïve cell. Clonal expansion: ~7 days. Effector response follows. Decreases until it becomes a memory cell. Memory cells persist and slowly decline after 14 days. Transcript Introduction0:00hello and welcome to another video in0:01this video I’m going to talk about the0:03t-lymphocytes development and functions0:05so let’s start with the development someT-Cell Development0:08bones in your body has what we call0:09yellow bone marrow consisting mainly of0:11fat cells and we also have spongy bone0:15what we call red bone marrow which is0:16very very vascular lead and in the red0:19bone marrow most of our red blood cells0:21and
Antigen Presenting Cells
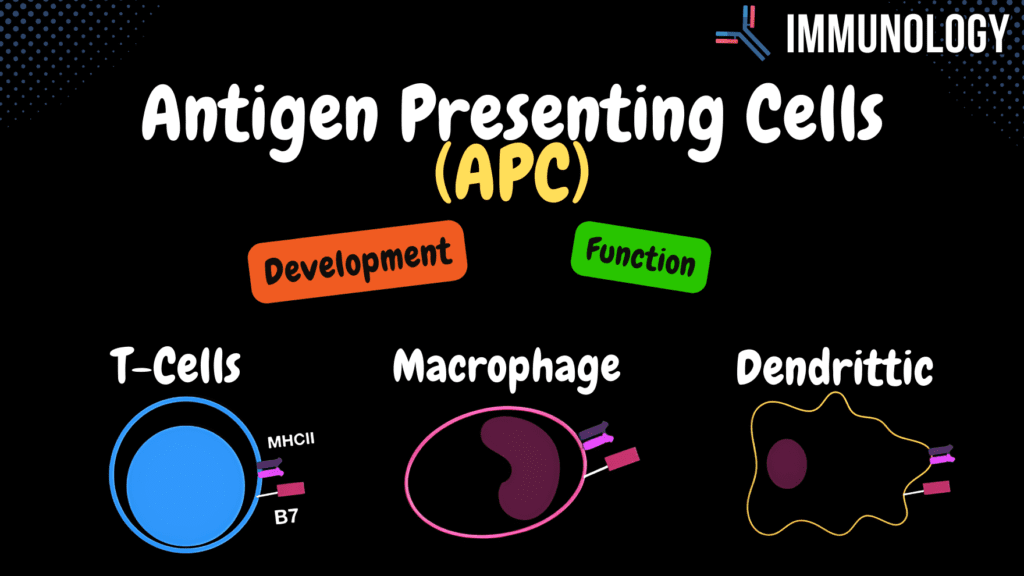
Antigen Presenting Cells (B-cells, Macrophage, Dendritic Cell) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript 📢 Currently, there is no PDF for this video.If you’re interested in having one, feel free to send an inquiry, and I may create it in the future. BUT! There’s a quiz available in the next tab. 12345678910 Antigen Presenting Cells – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 What type of immunity is mediated by antigen-presenting cells? A) Adaptive immunity B) Passive immunity C) Innate immunity D) Autoimmunity Antigen-presenting cells are involved in adaptive immunity by presenting antigens to T- and B-cells. 2 / 10 What cytokines are crucial for the differentiation of Th0 cells into Th1 cells? A) IL-10 B) IL-8 C) IL-4 D) IL-12 IL-12 released by macrophages is crucial for Th0 to Th1 differentiation. 3 / 10 What surface molecule on dendritic cells enhances their ability to activate T-cells? A) CD40 B) ICAM-1 C) MHC I D) B7 The B7 molecule on dendritic cells provides co-stimulatory signals to T-cells. 4 / 10 What is the function of B7 molecules on APCs? A) Presents antigens B) Provides co-stimulation C) Causes apoptosis D) Releases cytokines B7 provides the second activation signal to T-cells via interaction with CD28. 5 / 10 Where are B cells located in the lymph nodes? A) Germinal Center B) Cortex C) Medulla D) Paracortex B cells are primarily found in the outer cortex of the lymph nodes. 6 / 10 What happens when immature dendritic cells phagocytose antigens? A) Undergo apoptosis B) Become NK cells C) Migrate to lymph nodes D) Release cytokines Immature dendritic cells migrate to lymph nodes and express co-stimulatory molecules like B7. 7 / 10 What surface receptor on macrophages binds IgG-opsonized pathogens? A) CD40 B) MHC I C) Fc receptor D) TLR2 Fc receptors on macrophages bind to the Fc region of IgG, aiding in phagocytosis. 8 / 10 Which molecule on APCs provides the co-stimulatory signal to naive T-helper cells? A) MHC I B) B7 C) CD40 D) ICAM-1 The B7 molecule on APCs interacts with CD28 on T-helper cells to provide the second activation signal. 9 / 10 Which APC is located in epithelial tissues and migrates to lymph nodes upon activation? A) Macrophages B) B-Lymphocytes C) Langerhans Cells D) NK Cells Langerhans cells, a type of dendritic cell, are found in epithelial tissues and migrate to lymph nodes. 10 / 10 What cytokine is a major chemotactic factor released by activated macrophages? A) IL-1 B) IL-6 C) IL-8 D) TNF-alpha IL-8 is a key chemotactic factor for recruiting neutrophils and leukocytes. Your score is The average score is 0% Description This video is about Antigen Presenting Cells (APCs). All information in my immunology videos is sourced from: Book: Immunology, Eighth Edition by David Male, Jonathan Brostoff, David Roth, and Ivan Roitt Additional research: PubMed University lecture materials What Are Antigen Presenting Cells (APCs)? Phagocytose microorganisms and present them on MHC I or MHC II. Express B7 (Co-stimulatory molecule for T-cell activation). Present MHC II to naïve T-Helper Cells (CD4+). Require three activation signals to activate naïve T-helper cells: 1st Activation Signal: MHCII-TCR (CD4 and CD3) 2nd Activation Signal: B7 – CD28 3rd Activation Signal: Interleukins MHC I activates T-cytotoxic cells (CD8+). Professional Antigen Presenting Cells: B-Lymphocytes Macrophages Dendritic Cells Inactive/Unprofessional Antigen Presenting Cells: Langerhans Cells B-Lymphocytes: Produce antibodies against specific antigens. During development: B-cells randomly generate surface antibodies. If B-cells do not encounter antigens within a certain timeframe, they undergo apoptosis (Anergy). B-Lymphocyte Development: Occurs in the Spongy Bone: Starts as Pluripotent Hematopoietic Stem Cell. Pro B-Cell Pre B-Cell (Heavy chain recombination for IgM: VDJ gene) Immature B-Cell (Light chain recombination: VJ gene, IgM development complete) Mature B-Cell: Expresses both IgM and IgD on the surface. Checked for self-reactivity. If non-self-reactive → Travels to secondary lymphoid organs (Lymph nodes, spleen, Peyer’s patches). B-Lymphocyte Activation: B-Cell Receptor (BCR): Consists of IgD/IgM and signaling chains (Igα and Igβ). B-Cells reside in the outer cortex of lymph nodes. Steps: BCR binds to antigen. Endocytosis of BCR-antigen complex. Antigen is presented on MHC II to Th2 or Th0. Th2 binds to the activated B-cell through: CD40L-CD40 interaction TCR-MHCII interaction Cytokines (IL-4, IL-5, IL-10, IL-6, IL-2, IFN-γ) help B-cell differentiate. B-Cell becomes a Memory B-cell or Plasma Cell. T-cell Dependent B-cell Differentiation: Produces IgA, IgE, or IgG. T-cell Independent B-cell Differentiation: Rapidly produces IgM when polysaccharides bind to BCR (No memory B-cells produced). Macrophage Development: Pluripotent Hematopoietic Stem Cell Mono Stem Cell Pro-monoblast Monoblast Pro-monocyte Monocyte in blood Monocyte differentiates into: Free Macrophage (in tissue) Fixed Macrophage Dendritic Cell Macrophage Functions: MHC I and MHC II expression. Fc receptors: Fc IgG (Direct Opsonization) Fc IgE C3b receptor: Binds complement protein C3b. CD14: Recognizes Lipopolysaccharides (LPS). B7: Co-stimulation for T-cell activation. Active Macrophage Releases: Interleukin 12 (IL-12): Differentiates Th0 into Th1 and activates Natural Killer (NK) cells. Interleukin 8 (IL-8): Chemotaxis. Interleukin 1 (IL-1), IL-6, TNF-α: Act as endogenic pyrogens (cause fever). IL-1, IL-6, TNF-α travel to the hypothalamus → Release Prostaglandin E2 (PGE2). IL-6 travels to the liver → Causes the release of acute phase proteins. Dendritic Cells: Derived from monocytes in the blood. Highly migratory. Surface Markers: MHC I and MHC II B7 Adhesion molecules: Help bind T-lymphocytes. Langerhans Cells: Also known as immature dendritic cells. After phagocytosis, they migrate to lymph nodes and begin expressing B7. Transcript Introduction0:00hello and welcome to another video in0:01this video I’m gonna talk about the0:03different antigen presenting cells we0:05have in our body basically how they0:07develop and their characteristics soFunction of Antigen-Presenting Cells (APCs)0:10what is an antigen presenting cell these0:12cells are cells that can catch0:15microorganism and basically present them0:17on either MHC 1 or MHC 2 but these guys0:21were special with these guys is that0:23they can actually Express what is called0:24b7 and b7 is a major call simulator for0:28the T cells we have
Antibodies
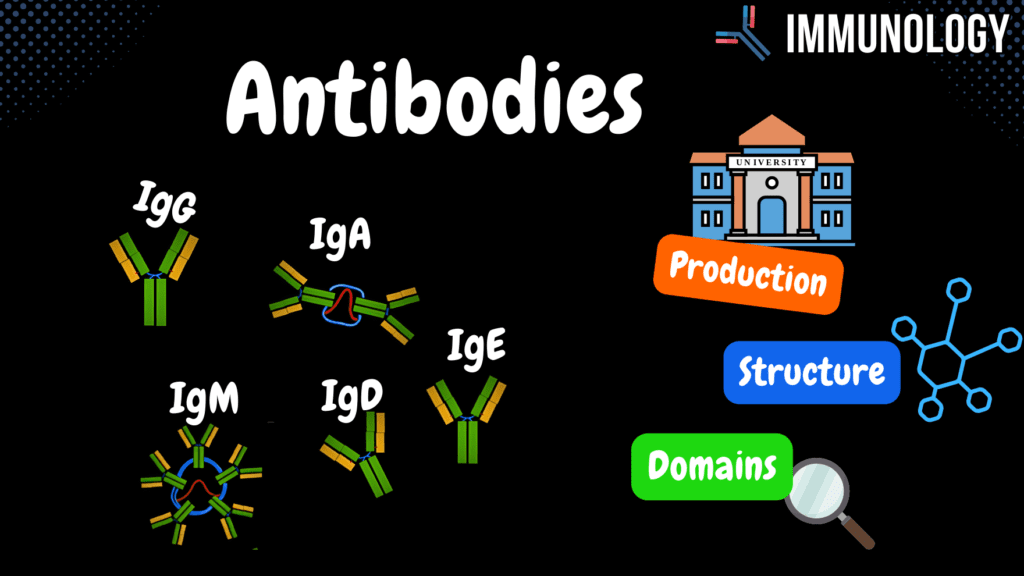
Antibodies (Origin, Components, Domains, IgG, IgM, IgA, IgD, IgE) + Table Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript 📢 Currently, there is no PDF for this video.If you’re interested in having one, feel free to send an inquiry, and I may create it in the future. BUT! There’s a quiz available in the next tab. 12345678910 Antibodies – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 What type of antibody diversity is determined by differences in the variable region? A) Idiotypic differences B) Conformational epitopes C) Allotypic differences D) Isotypic differences Idiotypic differences are based on variations in the variable region. 2 / 10 What determines the antigen-binding specificity of an antibody? A) Fab fragment B) Fc fragment C) Variable region D) Constant region The variable region of the light and heavy chains binds specifically to the antigen. 3 / 10 Which antibody is capable of crossing the placenta? A) IgG B) IgM C) IgE D) IgA IgG is the only antibody that can cross the placenta and provide passive immunity to the fetus. 4 / 10 Which antibody is predominantly found on the surface of immature B cells? A) IgA B) IgD C) IgG D) IgM IgD is primarily found on the surface of immature B cells. 5 / 10 What distinguishes T-cell-dependent from T-cell-independent antibody production? A) Produces diverse isotypes B) Produces IgD only C) Produces IgE only D) No memory formation T-cell-independent responses produce mainly IgM, while T-cell-dependent responses can produce all isotypes. 6 / 10 What is the primary role of IgA? A) Mucosal immunity B) Allergic response C) Complement activation D) Placental transfer IgA is primarily involved in mucosal immunity. 7 / 10 What is the structural form of IgM in the serum? A) Pentamer B) Monomer C) Dimer D) Trimer IgM exists as a pentamer in the serum, connected by a J-chain. 8 / 10 Which immunoglobulin is most effective in neutralizing toxins? A) IgA B) IgG C) IgM D) IgE IgG is highly effective in neutralizing toxins due to its specificity and abundance. 9 / 10 Which antibody isotype is primarily involved in allergic reactions? A) IgG B) IgM C) IgA D) IgE IgE is responsible for Type I hypersensitivity and allergic responses. 10 / 10 Which immunoglobulin is present in the highest concentration in plasma? A) IgE B) IgM C) IgA D) IgG IgG accounts for about 75% of antibodies in plasma. Your score is The average score is 0% Description This video is part 2 of Acquired Immunity – Antibodies. All information in my immunology videos is sourced from: Book: Immunology, Eighth Edition by David Male, Jonathan Brostoff, David Roth, and Ivan Roitt Additional research: PubMed University lecture materials Antibodies: Plasma Proteins Where They Come From: B-cell (with BCR – IgG/IgD) binds to an antigen. Presents it on MHC II. APC activates a naïve Th cell through: TCR (CD4 and CD3) B7/CD28 interaction IL-4 receptor Naïve T helper cell secretes IL-2 (autocrine). Becomes an active Th2. Th2 helps activate B-cells through CD40L/CD40 and T cell receptor. Cytokine release: IL-4, IL-5, IL-8, IL-10, IL-2, IFN-γ, depending on the required antibody type. Components of an Antibody: Light Chain Heavy Chain Variable Part Constant Region Antibody Structure: Divided into: Fab (Fragment Antigen Binding) Fc (Fragment Crystallizable Region) Contains: VL (Variable Light) VH (Variable Heavy) CL (Constant Light) CH1, CH2, CH3 (Constant Heavy regions) Connected through disulfide bonds. Hinge region allows antibody motility. Antibody Domains: Variable Region: Antigen binding site CH1 Region: Determines allotype CH2 Region: Binds complement CH3 Region: Binds cells Variants of Chains: Light Chain: Lambda Chain, Kappa Chain Heavy Chain: Gamma Chain (IgG) Mu Chain (IgM) Alpha Chain (IgA) Delta Chain (IgD) Epsilon Chain (IgE) Functions of Antibodies: IgG: Structure: Monomeric (with subtypes) Plasma Amount: 75% Only antibody that crosses the placenta. Direct opsonization. Activates the complement system. Primary antibody in the secondary immune response (produced by memory B-cells). IgM: Structure: Pentameric (with a J-chain), Monomeric on B-cells. Produced by fetal immune system. Acts as the primary response antibody but does not provide memory. Complement activation. IgA: Structure: Dimeric (J-chain), Monomeric, Trimeric. Located in mucosal areas (gut, respiratory tract, urogenital tract). Secreted by alpha plasma cells. Bound to epithelial cells via poly-IgA receptors. Transported through endocytosis and released by proteolytic cleavage. Some microorganisms can cleave IgA. IgD: Structure: Monomeric. Plasma Amount: Under 1%. Localized on B-cell surfaces. IgE: Structure: Monomeric. Plasma Amount: Very low. Function: Binds to mast cells. Responsible for Type I hypersensitivity (allergic reactions). Increased levels in allergic diseases and parasitic infections. Differences Between Immunoglobulins: Idiotypic Differences: Differ in variable region. Isotypic Differences: Differ in constant region. Allotypic Differences: Genetic variation between alleles of the same constant gene. Transcript Introduction0:00in this video we’re gonna look at0:01antibodies antibodies are plasma0:04proteins known as immunoglobulins now toWhere do Antibodies Come From?0:07understand the different immunoglobulins0:09we have in our body I feel like it’s0:11most natural to know where they come0:13from first right so we got our b-cells0:16right here right chillin in the cortex0:17of the lymph node I’ll show you a scheme0:19later B cells have was called b-cell0:21receptors on the surface composed of0:23either IgG or IgM antibodies which are0:26membrane bound and a single transducer0:29as a heterodimer called IgA and RGB0:31those are those transmit the signal to0:34the nucleus when the IgG or IgM binds to0:37something right so now let’s imagine0:40this antigen right here was just catched0:42from the interstitial fluid from the0:44lymph vessel and then brought to the0:46cortex of the lymph node and it was0:48unlucky enough to accent the fit to the0:51membrane bound antibody on the surface0:53of the B cell it’s then gonna perform an0:55antigen B cell receptor endocytosis and0:58present a fragment of the antigen an MHC1:02class 2 molecule remember b-cells are1:04also antigen presenting cells – at the1:07same time at the rate Excel can also1:08phagocyte and the antigen and eventually1:11presented an MHC class 2 molecule1:13remember generating cells and B cells1:15are
Acquired Immune System
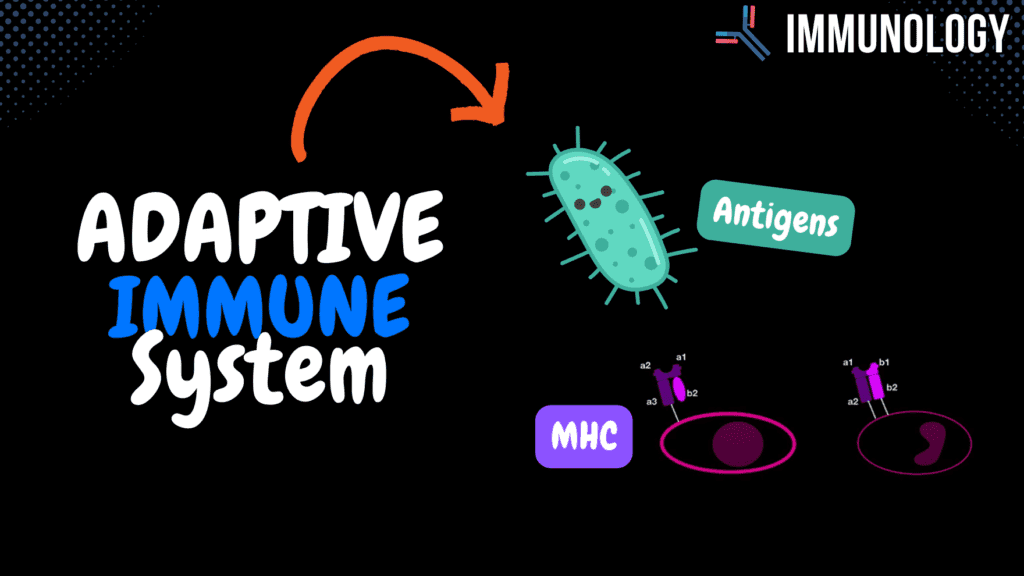
How the Acquired Immune System Work (Antigens, MHC) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript 📢 Currently, there is no PDF for this video.If you’re interested in having one, feel free to send an inquiry, and I may create it in the future. BUT! There’s a quiz available in the next tab. 12345678910 Acquired Immune System – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 What defines the ability of an antigen to elicit an immune response? A) Complement activation B) Epitope diversity C) Immunogenicity D) Antigenicity Immunogenicity defines the ability of an antigen to cause an immune response. 2 / 10 What does MHC Class I primarily present to cytotoxic T cells? A) Viral RNA B) Bacterial toxins C) Exogenous peptides D) Endogenous peptides MHC Class I presents endogenous peptides to cytotoxic T cells. 3 / 10 What gene encodes the human MHC complex? A) Complement genes B) Immunoglobulin genes C) Cytokine genes D) HLA The HLA (Human Leukocyte Antigen) genes on chromosome 6 encode the MHC complex. 4 / 10 Which class of MHC molecules is involved in presenting antigens to T-helper cells? A) MHC Class I B) MHC Class III C) Cytokine genes D) MHC Class II MHC Class II presents antigens to T-helper cells to activate the immune response. 5 / 10 What happens to cytotoxic T cells upon activation by MHC Class I? A) Release cytokines B) Neutralize antibodies C) Activate macrophages D) Kill infected cells Cytotoxic T cells kill infected cells via perforin and granzyme after activation. 6 / 10 Which component of MHC Class I interacts directly with CD8+ cytotoxic T cells? A) β2 domain B) α2 domain C) α3 domain D) β1 domain The α3 domain of MHC Class I interacts with CD8+ cytotoxic T cells. 7 / 10 Which antigen is associated with bacterial capsules? A) O-antigen B) Vi-antigen C) H-antigen D) K-antigen The K-antigen is associated with bacterial capsules. 8 / 10 Which cytokine is essential for T-helper cell differentiation into Th1 cells? A) IL-4 B) IL-12 C) IL-10 D) TNF-α IL-12 is essential for the differentiation of T-helper cells into Th1 cells. 9 / 10 What triggers the activation of naïve T cells in lymph nodes? A) NK cell activation B) Antibody binding C) Antigen presentation D) Complement activation Antigen presentation by professional APCs via MHC molecules triggers T-cell activation. 10 / 10 What is the primary function of MHC Class III molecules? A) Encode complement proteins B) Induce fever C) Present antigens D) Activate B cells MHC Class III encodes complement proteins and cytokines, but does not present antigens. Your score is The average score is 0% Description This video is Part 1 of Acquired Immunity – Antigens and MHC. All information in my immunology videos is sourced from: Book: Immunology, Eighth Edition by David Male, Jonathan Brostoff, David Roth, and Ivan Roitt Additional research: PubMed University lecture materials Difference Between Innate and Acquired Immunity: Innate Immunity: Non-specific No immunological memory Attacks all agents equally Acquired Immunity: Specific defense Develops immunological memory Two Types of Acquired Immunity: Active Acquired Immunity: Developed through natural infection by microorganisms Induced through vaccination Outcome: Long-lasting immunity and antibody production Passive Acquired Immunity: Acquired by receiving antibodies (e.g., injection of antibodies) Transferred from mother to fetus through the placenta Outcome: Temporary immunity, as antibodies are used up over time Two Ways Adaptive Immunity Works: Humoral Immune Response: Antimicrobial Antiviral Antitoxic Cellular Immune Response: Attacks infected cells directly Antigens: Microorganisms Red Blood Cells Oncogenic Cells (Cancer Cells) Virus-Infected Cells Toxins and Venoms Proteins (Most immunogenic) Polysaccharides Lipoproteins Immunogenicity vs. Antigenicity: Immunogenicity: Ability to induce an immune response Antigenicity: Ability to bind to an antibody Epitopes: Multivalent antigen with different epitopes Multivalent antigen with repeated epitopes Continuous/Linear Epitopes Discontinuous/Conformational Epitopes Types of Antigens: Complete Antigen: Can induce an immune response Incomplete Antigen: Can bind to antibodies but does not trigger an immune response Thymus-Dependent Antigen: Requires T-helper cells for activation Thymus-Independent Antigen: Can activate B cells without T-helper cells Major Histocompatibility Complex (MHC): Human Leukocyte Antigens (HLA): MHC in humans Gene Location: Chromosome 6 (short arm) MHC Classification: MHC Class I: Includes HLA-A, HLA-B, HLA-C Present on all nucleated cells Structure: Alpha chain (1, 2, 3) and Beta chain 2 MHC Class II: Includes HLA-DR, HLA-DQ, HLA-DP, HLA-DM Present on professional antigen-presenting cells Structure: Alpha chains (1, 2) and Beta chains (1, 2) MHC Class III: Codes for complement proteins (C2, C4, Factor B) and cytokines MHC Class I Function: Recognized by: Natural Killer (NK) cells and Cytotoxic T cells (CD8+ T cells) Normal Function: Displays self-peptides on MHC I for immune surveillance Infected Cells: Present altered peptides on MHC I Recognized and destroyed by Cytotoxic T cells using Granzyme B and Perforin NK Cells: Recognize and kill cells with decreased MHC I expression MHC Class II Function: Antigen-Presenting Cells (APCs): Present foreign peptides to T-helper cells (CD4+ T cells) Leads to immune system activation Group Antigens: Enterobacteriaceae (E. coli, S. typhi): Different bacterial species share common antigens Antigen Types: O-Antigen: Lipopolysaccharides Vi-Antigen: Virulence factors K-Antigen: Capsular antigen H-Antigen: Flagellar antigen Transcript Introduction0:00hello and welcome to another video in0:02this video I’m going to talk about0:03acquired immunity now the immune system0:06uses two main strategies to defeat any0:08type of unwanted invaders one of them is0:10called the innate and other ones called0:12acquired so the innate immune system is0:14mainly present since birth and therefore0:16sometimes also called the natural immune0:19system they acquired however forms0:21during a person’s lifetime and it’s0:23therefore sometimes also called adaptive0:24now please don’t get this wrong this0:26baby also has some type of acquired0:28immune system I just put it there to0:29show you that you’ve always had innate0:32immune system ever since you were born0:33all right so let’s put this to practice0:36imagine there are three different types0:37of bacterias right the Indian immune0:40system is what we call nonspecific0:42because it’s going to attack all of0:43these
Complement System
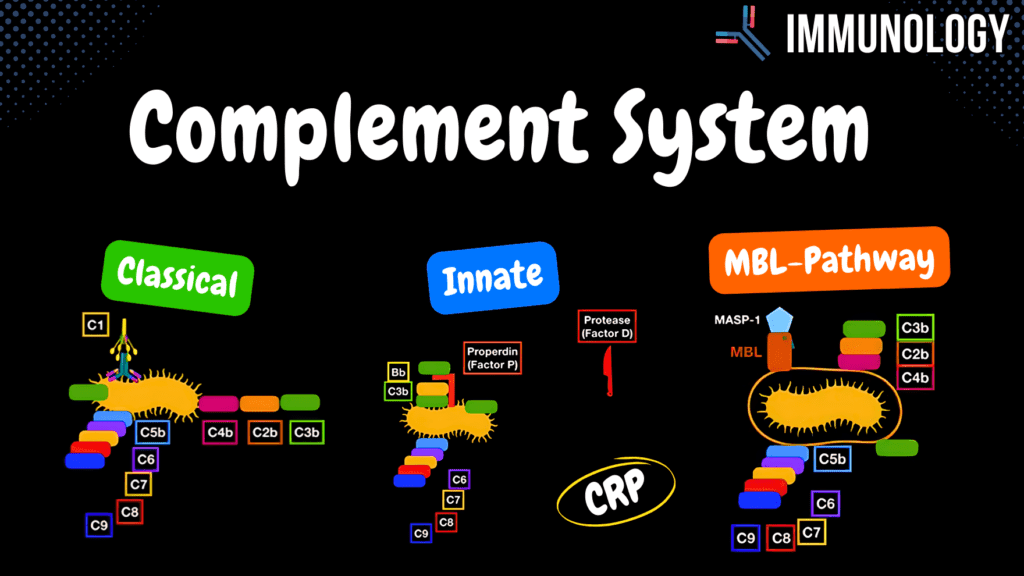
Complement System Pathways (Classical, Alternative, MBL) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript 📢 Currently, there is no PDF for this video.If you’re interested in having one, feel free to send an inquiry, and I may create it in the future. BUT! There’s a quiz available in the next tab. 12345678910 Complement System – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 Which cytokine is responsible for acute phase protein production in the liver during infection? A) IL-6 B) TNFα C) IL-1 D) IL-8 IL-6 induces the production of acute phase proteins like CRP and MBL in the liver. 2 / 10 What triggers the Mannose Binding Lectin pathway of complement activation? A) MBL binding to mannose B) Antibodies binding C) C3 spontaneous cleavage D) Acute phase proteins Mannose Binding Lectin binds to mannose residues on the surface of pathogens like fungi. 3 / 10 Which complement factor amplifies the classical pathway by forming a feedback loop? A) C4a B) C3b C) C5a D) Properdin C3b amplifies the classical pathway by enhancing the formation of C5 convertase. 4 / 10 What is the function of the C3 convertase enzyme in the complement system? A) Cleaves C3 B) Activates cytokines C) Neutralizes toxins D) Forms MAC C3 convertase cleaves C3 into C3a and C3b, initiating further amplification of the complement cascade. 5 / 10 What is the main trigger for the lectin pathway of complement activation? A) Antibodies B) C3 spontaneous cleavage C) MBL binding D) Cytokine release Binding of Mannose Binding Lectin (MBL) to mannose residues on pathogens activates the lectin pathway. 6 / 10 Which complement pathway does not lead to the formation of a Membrane Attack Complex (MAC) on capsules? A) Classical Pathway B) Mannose Binding Lectin Pathway C) Lectin Pathway D) Alternative Pathway The Mannose Binding Lectin pathway does not form a MAC on capsules, as it targets exposed mannose residues. 7 / 10 What is the role of C1q in the classical pathway of complement activation? A) Binds antibodies B) Activates cytokines C) Forms C5 convertase D) Cleaves C4 C1q binds to the Fc region of antibodies attached to pathogens, initiating the classical pathway. 8 / 10 What is the significance of MASP-1 in the Mannose Binding Lectin pathway? A) Stabilizes C3 convertase B) Activates cytokines C) Acts as a serine protease D) Forms MAC MASP-1 binds to MBL and acts as a serine protease to cleave complement proteins. 9 / 10 What is the role of anaphylatoxins like C3a, C4a, and C5a in the immune response? A) Promotes antigen presentation B) Increase vascular permeability C) Neutralizes antigens D) Forms Membrane Attack Complex Anaphylatoxins increase capillary permeability and activate mast cells, contributing to inflammation. 10 / 10 What is the role of C3a in the complement cascade? A) Neutralizes antigens B) Forms C5 convertase C) Anaphylatoxin D) Activates MAC C3a acts as an anaphylatoxin, promoting inflammation by increasing vascular permeability and activating mast cells. Your score is The average score is 0% Description This video is part 3 of Innate Immunity – Complement System (Humoral Factors). All information in my immunology videos is sourced from: Book: Immunology, Eighth Edition by David Male, Jonathan Brostoff, David Roth, and Ivan Roitt Additional research: PubMed University lecture materials Mechanisms of the Complement System: Membrane Attack Complex (MAC) Chemotaxis Opsonization Anaphylatoxins Classical Pathway: Antibody-dependent (Adaptive Immune System) Step 1: C1q binds to antibody-antigen complex Step 2: C1r activates C1s Step 3: C1s cleaves C4 and C2 Step 4: C4b and C2b form C3 convertase Step 5: C3 convertase cleaves C3, which binds to the surface as an opsonin or binds to C3 convertase to form C5 convertase Step 6: Membrane Attack Complex (MAC) forms on Gram-negative bacteria Alternative Pathway: Antibody-independent Step 1: C3 undergoes spontaneous cleavage in the bloodstream. C3b binds to bacterial surfaces Step 2: Factor B binds Step 3: Factor D cleaves Factor B into Bb Step 4: Properdin (Factor P) stabilizes the complex, forming C3 convertase Step 5: The pathway proceeds as in the classical pathway Mannose-Binding Lectin (MBL) Pathway: Triggered by Acute Phase Response Step 1: Active macrophages release IL-1, IL-6, and TNF-α as endogenous pyrogens Step 2: Cytokines travel to the hypothalamus, triggering Prostaglandin E2 (PGE2) release and causing fever Step 3: IL-6 signals the liver to release acute phase proteins, including C-reactive protein (CRP) and Mannose-Binding Lectin (MBL) C-Reactive Protein (CRP) Functions: Acts as an opsonin Activates the classical pathway of the complement system Mannose-Binding Lectin (MBL) Pathway: Activation begins 1-2 days after infection Step 1: MBL binds to Mannose (monosaccharide) on fungal capsules and surfaces Step 2: MBL recruits MASP-1 (Mannan-binding Lectin Serine Protease 1), which functions as an enzyme Step 3: The pathway proceeds as in the classical pathway Note: The Membrane Attack Complex (MAC) does not form on capsules. Complement System Effector Functions: C4a, C5a, and C3a: Act as Anaphylatoxins by increasing capillary permeability and activating mast cells Function in Chemotaxis by directing phagocytes to infection sites Complement system removes immune complexes from the bloodstream Transcript Introduction0:00the compliment system is a part of the0:02immune system that enhances the defense0:04against pathogens and there are0:06different mechanisms that the complement0:08system actually has that allows it to0:10help the immune system one of these ways0:13is that it forms this complex on the0:15surface of the micro organisms called0:17the membrane attack complex which makes0:19holes on the membrane of the micro0:21organisms and these holes going to0:23disturb the environment inside the cell0:26by water leaking in causing cell lysis0:29so what more can I do you know when a0:32macrophage is just circling around your0:33body the complement system acts as0:36something called chemotaxis where they0:38go tell the macrophage hey I found a0:40bacteria can come and kill it hence I0:42underlined the word taxi because it0:44actually works at a taxi for the0:45macrophages it tells them where to go0:47all the things we can do is work as0:49obstinate and optimize
Innate Immune System
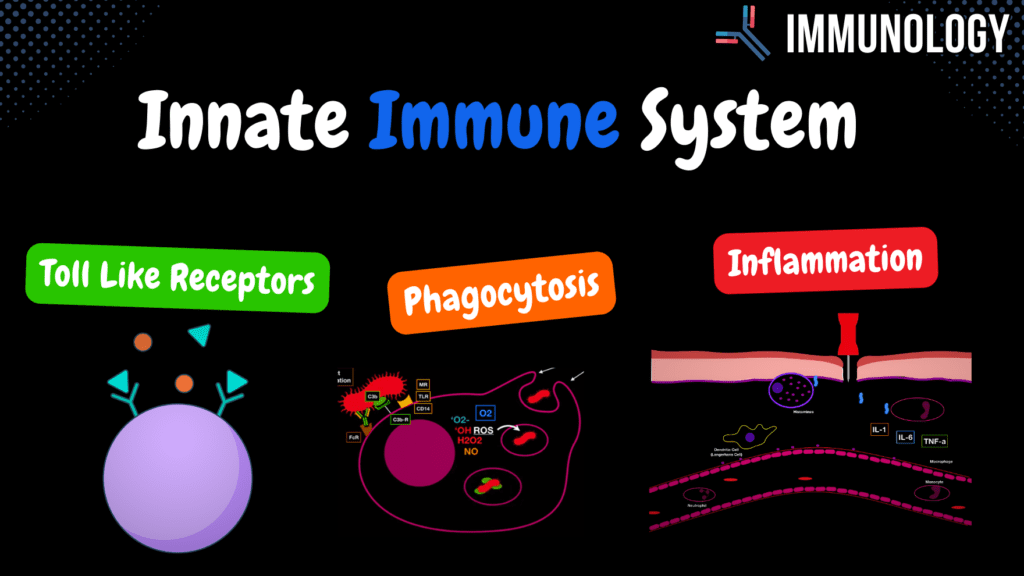
Innate Immune System (Toll Like Receptors, Phagocytosis & inflammation ) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript 📢 Currently, there is no PDF for this video.If you’re interested in having one, feel free to send an inquiry, and I may create it in the future. BUT! There’s a quiz available in the next tab. 12345678910 Innate Immune System (Inflammation) – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 What is the role of TNFα during inflammation? A) Neutralizes toxins B) Activates NK cells C) Enhances phagocytosis D) Activates endothelial cells TNFα activates endothelial cells and contributes to vascular permeability. 2 / 10 Which Toll-Like Receptor (TLR) recognizes unmethylated CpG islands in bacterial DNA? A) TLR3 B) TLR7 C) TLR9 D) TLR4 TLR9 recognizes unmethylated CpG DNA, which is common in bacterial genomes. 3 / 10 Which Toll-Like Receptor (TLR) is involved in recognizing bacterial lipopolysaccharides (LPS)? A) TLR4 B) TLR1 C) TLR3 D) TLR5 TLR4 recognizes LPS, a component of gram-negative bacterial cell walls. 4 / 10 Which Toll-Like Receptor (TLR) recognizes single-stranded viral RNA? A) TLR3 B) TLR9 C) TLR5 D) TLR7 TLR7 recognizes single-stranded RNA from viruses, triggering an antiviral response. 5 / 10 Which step in phagocytosis involves the fusion of a phagosome with a lysosome? A) Formation of phagolysosome B) Binding C) Engulfment D) Antigen presentation The fusion of a phagosome with a lysosome leads to the formation of a phagolysosome for pathogen digestion. 6 / 10 What is the role of reactive oxygen species (ROS) in phagocytosis? A) Bind to PAMPs B) Neutralize toxins C) Activate complement D) Kill pathogens ROS mediate oxygen-dependent killing of engulfed pathogens. 7 / 10 Which cells are classified as professional phagocytes? A) Neutrophils B) B cells C) Plasma cells D) NK cells Neutrophils, macrophages, dendritic cells, and mast cells are professional phagocytes. 8 / 10 What is the role of opsonization in phagocytosis? A) Activate complement system B) Secrete cytokines C) Enhance pathogen binding D) Neutralize toxins Opsonization enhances pathogen binding by marking them for phagocytosis with antibodies or complement proteins. 9 / 10 What is the role of macrophages in antigen presentation? A) Secrete complement B) Neutralize toxins C) Present antigens to T cells D) Produce antibodies Macrophages present antigens to T cells using MHC class I or II molecules. 10 / 10 What is the role of lysosomes in phagocytosis? A) Digest pathogens B) Release cytokines C) Bind pathogens D) Present antigens Lysosomes release enzymes for oxygen-independent digestion of pathogens. Your score is The average score is 0% Description This video is part 2 of Innate Immunity – Cellular Factors (Toll-like Receptors, Phagocytosis, and Inflammation). All information in my immunology videos is sourced from: Book: Immunology, Eighth Edition by David Male, Jonathan Brostoff, David Roth, and Ivan Roitt Additional research: PubMed University lecture materials TLR dimerization: Link Toll-like Receptors (TLRs): Location: Epithelial Cells of the mucous membrane Endothelial Cells Macrophages Dendritic Cells Neutrophils Membrane-bound TLRs: TLR 1/2 and TLR 2/6: Recognize Peptidoglycan/Lipoteichoic acid, Lipoproteins TLR 4: Recognizes Lipopolysaccharides, Fungal Mannan, Viral Envelope Proteins TLR 5: Recognizes Bacterial Flagellin Intracellular Receptors: TLR 3: Recognizes Double-stranded RNA from viruses TLR 7: Recognizes Single-stranded RNA TLR 8: Recognizes Double-stranded RNA from viruses TLR 9: Recognizes Unmethylated CpG islands Toll-like Receptors trigger: Release of cytokines (TNF, IL-1, IL-12) Release of chemokines (IL-8) Release of antiviral cytokines (IFN α/β) Phagocytosis: Professional Phagocytes: Neutrophils Macrophages/Monocytes Mast Cells Dendritic Cells Steps in Phagocytosis: Binding: Non-specific surface receptors (Mannose Receptor, Toll-like Receptor, CD14), Indirect Opsonization (C3b), Direct Opsonization (Fc receptor to antibody) Engulfment: Pseudopods wrap around the bacteria Phagosome Formation: Enclosure of the pathogen within a vesicle Digestion: Oxygen-dependent digestion (Reactive Oxygen Species) Oxygen-independent digestion Lysosome: Breaks down bacterial cell walls Enzymes: Proteolytic and hydrolytic enzymes Antimicrobial peptides (Defensins) Acidic reactions (low pH) Lactoferrin (in neutrophils) Antigen Presentation: Presented on MHC class I or II, or released into interstitial fluid to be absorbed by lymph vessels Macrophage Cytokine Release: Interleukin 8: Chemotaxis for Leukocytes Interleukin 1: Activates T-Lymphocytes and Macrophages Interleukin 6: Activates T- and B-Lymphocytes TNF-α: Activates Endothelium Interleukin 12: Activates Natural Killer Cells Endogenic Pyrogens (Fever Induction): IL-1, IL-6, TNF-α stimulate the hypothalamus to release Prostaglandins E2 IL-6 stimulates the liver to release acute phase proteins Incomplete Phagocytosis: Some bacteria evade digestion: Listeria: Releases Listeriolysin to escape phagosomes Mycobacterium tuberculosis: Produces catalase to resist degradation Immune System in Inflammation: Swelling: Due to increased permeability of blood vessels Pain: Due to diapedesis and edema pressing on pain receptors Heat: Due to increased blood flow Redness: Caused by vasodilation Transcript Introduction 0:00 and the last video we looked at the 0:01 general factors in the innate immune 0:03 system now we’re going to look at the 0:05 cellular factors in the immune system 0:07 which generally includes the taluk 0:09 receptors the phagocytosis and 0:10 inflammation natural killer cells and 0:13 the microbiota also a part of the 0:15 cellular factors keep that in mind so 0:18 we’ll start with Tullock receptors Toll-Like Receptors 0:20 toddler preceptors are receptors you 0:22 don’t really hear about so much but 0:25 they’re actually a really important part 0:27 of the body’s nonspecific resistance and 0:29 they’re really good at activating both 0:31 innate and adaptive immunity you will 0:34 find these receptors on specific areas 0:36 in your body you will find them lining 0:38 the epithelial cells of the mucous 0:40 membranes at portland’s of entry this 0:43 includes the MCOs of the nasal cavity 0:44 the mouth esophagus lungs and many more 0:47 you will also find them lining in detail 0:50 yourselves of the blood vessels this is 0:52 very very crucial because it helps the 0:54 body detect microorganisms very fast and 0:57 you won’t just find them on tissue 0:58 you’ll also find them in cells of the 1:01 first line of defense like
Innate Immune System Overview
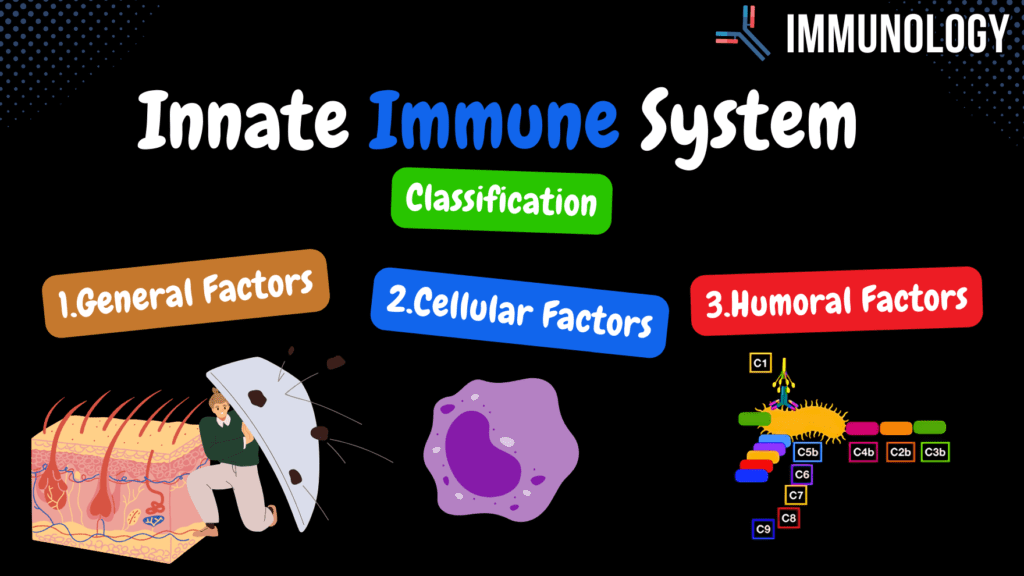
Innate Immune System: Simple Overview (Classification, General Factors) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript 📢 Currently, there is no PDF for this video.If you’re interested in having one, feel free to send an inquiry, and I may create it in the future. BUT! There’s a quiz available in the next tab. 12345678910 Innate Immune System Overview – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 What is the purpose of the complement system in innate immunity? A) Decreases inflammation B) Stimulates fever C) Enhances phagocytosis D) Activates NK cells The complement system enhances phagocytosis, promotes inflammation, and directly lyses pathogens. 2 / 10 Which cellular factor in innate immunity destroys pathogens via engulfment? A) NK cells B) TLRs C) Phagocytes D) Complement proteins Phagocytes, like macrophages, engulf and destroy pathogens. 3 / 10 What innate immune process directly lyses pathogens? A) Toll-like receptors B) Complement system C) NK cells D) Defensins The complement system lyses pathogens by forming membrane attack complexes. 4 / 10 What role do natural killer cells play in innate immunity? A) Destroy infected cells B) Neutralize toxins C) Activate PAMPs D) Secrete lysozyme NK cells identify and destroy infected or abnormal cells without prior activation. 5 / 10 What substance secreted by mucous membranes destroys bacterial cell walls? A) Interferons B) Lysozyme C) Defensins D) Pepsin Lysozyme, secreted by mucous membranes, destroys bacterial cell walls to protect against infection. 6 / 10 What do defensins secreted by mucous membranes do? A) Stimulate inflammation B) Disrupt pathogen membranes C) Neutralize toxins D) Activate complement Defensins are antimicrobial peptides that disrupt the membranes of pathogens. 7 / 10 What distinguishes innate immunity from acquired immunity? A) Specific, gains memory B) Non-specific, no memory C) Non-specific, gains memory D) Specific, no memory Innate immunity is non-specific and lacks immunological memory, attacking all agents equally. 8 / 10 Which general factor of innate immunity is influenced by pyrogenic reactions? A) Complement system B) Skin C) Fever D) Phagocytosis Pyrogenic reactions like fever are general factors that help fight infections by raising body temperature. 9 / 10 Which innate immune component detects and binds PAMPs? A) Lysozyme B) NK cells C) Complement proteins D) Toll-like receptors Toll-like receptors (TLRs) detect and bind pathogen-associated molecular patterns (PAMPs). 10 / 10 Which innate immune component directly attacks viral infections? A) Interferons B) Complement system C) Lysozyme D) Phagocytosis Interferons are proteins that interfere with viral replication and activate immune responses. Your score is The average score is 0% Description This video is part 1 of Innate Immunity – Classification and General Factors. All information in my immunology videos is sourced from: Book: Immunology, Eighth Edition by David Male, Jonathan Brostoff, David Roth, and Ivan Roitt Additional research: PubMed University lecture materials Difference between Innate and Acquired Immunity: Innate Immunity: Non-specific No immunological memory Attacks all agents equally Acquired Immunity: Specific defense Gains immunological memory Classification of Innate Immunity: General Factors: Barriers (Skin and Gastrointestinal tract) Pyrogenic reactions (Fever) Secretion Cellular Factors: Microbiota Phagocytosis Natural Killer Cells Toll-like Receptors Inflammatory reaction Humoral Factors: Complement System Interferons General Factors: Skin: Physical barrier due to tight junctions Secretion of antimicrobial products Mucous Membranes: Contain antimicrobial substances such as lysozyme, pepsin, and defensins Low pH provides additional protection Transcript Introduction0:00hello and welcome to another video this0:02video is mainly going to be about the0:03innate immune system now your immune0:06system uses two main strategies to0:08defeat any type of unwanted invaders one0:11of the strategies is called the innate0:12immune system and the other ones called0:14acquired immune system the innate immune0:16system is mainly present since birth and0:18is therefore sometimes also called the0:20natural immune system0:21well they acquired however forms during0:23a person’s lifetime and is therefore0:25sometimes also called the adapted now0:27just remember that the baby also has0:30some type of acquired immune system I0:31just put the baby there to show you that0:33you’ve always had the innate immune0:35system ever since you were born so now0:37let’s put this to practice imagine we0:39have three different types of bacteria0:40right the innate immune system is what0:43we call nonspecific because it actually0:46works against any type of agents equally0:48the adaptive however works very specific0:52as you see right here and not only that0:55upon defeating the bacteria you gain0:57some kind of immunological memory which0:59usually becomes enhanced upon repeated1:02exposure to the same agents the innate1:05immunity doesn’t really have that as1:06well let’s see how that works we mainlyClassification of the Innate Immune System1:09classify the immune system into three1:11different types the first is well called1:13general factors and we’ve got the1:15cellular factors and also have the1:17humoral factors the general factors1:20include physiological barriers at the1:23portal of entry like the skin and the1:25mucous membranes and they’re usually1:28analogically enough the first line of1:30defense next we have the para genetic1:33reactions now don’t get scared if you1:34haven’t heard this term before I’ll get1:36more into this later on talk about the1:38macrophages mainly but pyrogenic1:41reactions often refer to as fever some1:45viruses and bacterias cannot really1:47replicate optimally because the body1:49changes its temperature so that’s why we1:52call it the general factors because it1:55works generally by increasing the1:56temperature another general factors are2:00secretion inab secretion of different2:02enzymes fatty acids the cellular factors2:05we got your own microbiota fighting for2:07space and food the phagocytosis by cells2:11like neutrophils and macrophages2:13they do that by the different receptors2:16they have in the surface I also got2:18natural killer cells so they’re really2:19important for the antiviral immune2:21response these cells can bind to surface2:25of antigens by using toll-like receptors2:27which usually to inflammatory response2:30you also get humoral factors which2:32include the complement system at the2:34interference now I know this seems a lot2:36but trust me it all gets logical once2:39you understand the concept in my opinion2:41if you want to learn immunology properly2:43you need to understand different parts2:46individually before you can understand2:49the whole concept together in in system2:51and that’s what I’m aiming to show you2:54everything individually first and then2:56put them all together and show you have2:58this wort in the system alright so inGeneral
