Subclavian Artery
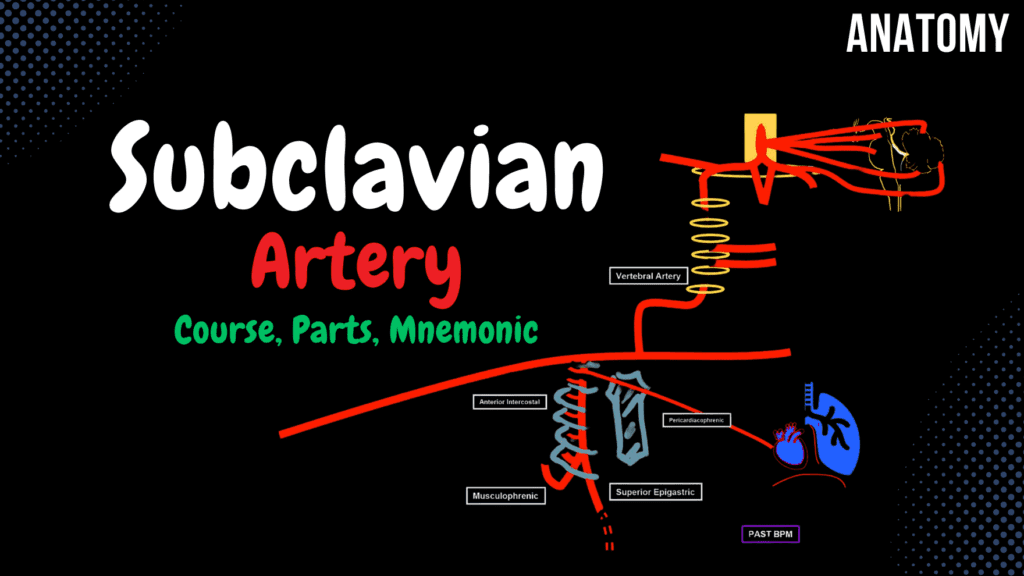
Subclavian Artery Scheme (Course, Branches, Parts, Mnemonics) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript Notes ☆ Member Only Go to PDF Notes Illustrations ☆ Member Only Go to Illustrations 12345678910 Subclavian Artery – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 Which branch of the subclavian artery gives rise to the superior epigastric artery? A) Thyrocervical trunk B) Vertebral artery C) Supreme intercostal artery D) Internal thoracic artery The internal thoracic artery gives rise to the superior epigastric artery, which supplies the anterior abdominal wall. 2 / 10 Which branch of the subclavian artery supplies the thyroid gland and the cervical esophagus? A) Dorsal scapular artery B) Vertebral artery C) Inferior thyroid artery D) Supreme intercostal artery The inferior thyroid artery, a branch of the thyrocervical trunk, supplies the thyroid gland and cervical esophagus. 3 / 10 Which artery arises from the thyrocervical trunk and participates in the scapular anastomosis? A) Vertebral artery B) Dorsal scapular artery C) Transverse cervical artery D) Suprascapular artery The suprascapular artery, a branch of the thyrocervical trunk, participates in the scapular anastomosis. 4 / 10 Which artery gives rise to the superior epigastric and musculophrenic arteries? A) Thyrocervical trunk B) Vertebral artery C) Internal thoracic artery D) Costocervical trunk The internal thoracic artery branches into the superior epigastric and musculophrenic arteries to supply the abdominal wall and diaphragm. 5 / 10 Which branch of the subclavian artery supplies the anterior thoracic wall and diaphragm? A) Thyrocervical trunk B) Vertebral artery C) Supreme intercostal artery D) Internal thoracic artery The internal thoracic artery arises from the first part of the subclavian artery and supplies the anterior thoracic wall and diaphragm. 6 / 10 Which branch of the subclavian artery supplies the scapula and posterior shoulder region? A) Suprascapular artery B) Dorsal scapular artery C) Transverse cervical artery D) Vertebral artery The suprascapular artery, a branch of the thyrocervical trunk, supplies the scapula and posterior shoulder region. 7 / 10 Which clinical condition results from compression of the subclavian artery at the thoracic outlet? A) Thoracic outlet syndrome B) Subclavian steal syndrome C) Raynaud's phenomenon D) Arterial embolism Thoracic outlet syndrome occurs when the subclavian artery is compressed, leading to ischemic symptoms in the upper limb. 8 / 10 Which branch of the subclavian artery forms part of the scapular anastomosis? A) Internal thoracic artery B) Dorsal scapular artery C) Thyrocervical trunk D) Costocervical trunk The dorsal scapular artery forms part of the scapular anastomosis and supplies the rhomboid and levator scapulae muscles. 9 / 10 Which branch of the costocervical trunk supplies the deep neck muscles? A) Vertebral artery B) Internal thoracic artery C) Thyrocervical trunk D) Deep cervical artery The deep cervical artery, a branch of the costocervical trunk, supplies the deep neck muscles. 10 / 10 Which branch of the subclavian artery ascends to supply the brain and spinal cord? A) Internal thoracic artery B) Supreme intercostal artery C) Thyrocervical trunk D) Vertebral artery The vertebral artery ascends through the transverse foramina of the cervical vertebrae to supply the brain and spinal cord. Your score is The average score is 0% Description This video will cover: Branches of the Subclavian Artery Subclavian Artery Right Subclavian Artery arises from the Brachiocephalic Trunk. Left Subclavian Artery arises directly from the Aorta. Subclavian Artery Mnemonic: VIT. C, D (as in VITamin C, D) 1st Part of the Subclavian Artery Vertebral Artery Prevertebral Part Transverse Part: Muscular Branch – supplies deep muscles of the neck. Spinal Branch – supplies upper 5th-6th cervical segments of the spinal cord. Intracranial Part: Anterior Spinal Artery – descends along the anterior median fissure. Posterior Spinal Arteries – descend along the posterolateral sulcus. Inferior Posterior Cerebellar Artery. Meningeal Branch – supplies the posterior meninges. Basilar Artery: Inferior Anterior Cerebellar Artery. Superior Cerebellar Artery. Branches for the pons and mesencephalon (midbrain). Posterior Cerebral Artery. Internal Thoracic Artery Divides into: Superior Epigastric Artery – passes through the sternocostal triangle and anastomoses with the Inferior Epigastric Artery. Musculophrenic Artery – gives off anterior intercostal arteries for the lower 5th-6th intercostal spaces. Mnemonic for Branches of the Internal Thoracic Artery: PAST BPM Pericardiophrenic artery Anterior intercostal artery Sternal artery Thymic artery Bronchial artery Perforating artery Mediastinal artery Thyrocervical Trunk Inferior Thyroid Artery Inferior Laryngeal Branch. Tracheal Branch. Esophageal Branch. Pharyngeal Branch. Ascending Cervical Artery Muscular Branch. Spinal Branches. Suprascapular Artery Transverse Cervical Artery Superficial Cervical Artery. Dorsal Scapular Artery (may arise from the Transverse Cervical or directly from the Subclavian Artery in the 3rd part). 2nd Part of the Subclavian Artery Costocervical Trunk Deep Cervical Artery. Supreme Intercostal Artery. Posterior Intercostal Arteries. 3rd Part of the Subclavian Artery Dorsal Scapular Artery (may arise from the Subclavian Artery or from the Transverse Cervical Artery). Sources Used: Memorix Anatomy (2nd Edition) – Hudák Radovan, Kachlík David, Volný Ondřej. Complete Anatomy by 3D4Medical. Biorender. University Notes and Lectures. Transcript Introduction0:00all right so this video will be about0:01two subclavian artery I will try to0:03cover it briefly and throw in a fume0:05demonics for you to remember so let’s do0:08a quick overview starting with the heart0:10and the I will talk with these three0:12branches the left common carotid artery0:14the left subclavian and the0:16brachiocephalic trunk which divides in0:18the right common carotid artery and the0:20right subclavian artery now remember0:23this that the left subclavian artery is0:25directly from the outer while the right0:28one comes from the breath use of0:29electrons one way to remember this is0:32that the outer curves to the left before0:34it descends right so it doesn’t really0:37need those extra centimetres that’s0:38provided by the brachiocephalic trunk0:40that’s just how I remember that the left0:42subclavian is directly from the outer so0:46the rest of this video will be on the0:48right subclavian but keep in mind that0:50everything you find on the right0:52subclavian artery will also be on the0:54left subclavian artery as well the only0:56difference is is that the left’s artery0:58is roughly around four
Blood Supply of the Eye
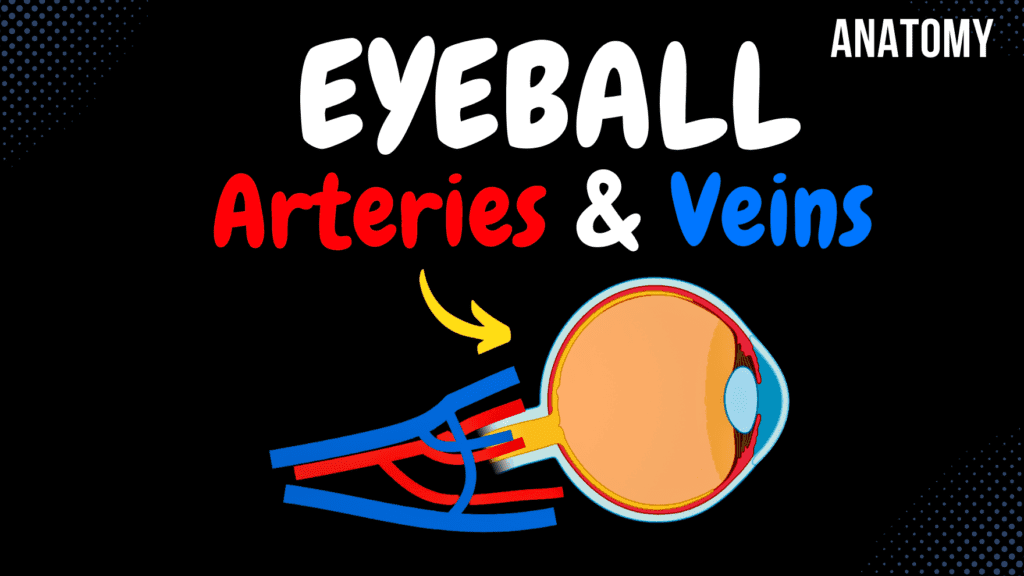
Blood Supply of the Eye Scheme (Ophthalmic Artery & Vein) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript Notes ☆ Members Only Go to PDF Notes Illustrations ☆ Members Only Go to Illustrations 12345678910 Blood Supply of the Eye – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 Which branch of the ophthalmic artery supplies the skin of the medial forehead? A) Supratrochlear artery B) Dorsal nasal artery C) Lacrimal artery D) Supraorbital artery The supratrochlear artery supplies the skin and muscles of the medial forehead. 2 / 10 Which branch of the ophthalmic artery supplies the forehead? A) Supratrochlear artery B) Lacrimal artery C) Supraorbital artery D) Dorsal nasal artery The supraorbital artery supplies the forehead and scalp. 3 / 10 What forms the inferior palpebral arch? A) Supraorbital artery B) Supratrochlear artery C) Medial and lateral palpebral arteries D) Central retinal artery The inferior palpebral arch is formed by the medial and lateral palpebral arteries. 4 / 10 Which artery supplies the lacrimal gland? A) Lacrimal artery B) Supraorbital artery C) Ethmoidal artery D) Dorsal nasal artery The lacrimal artery supplies the lacrimal gland and contributes to the lateral palpebral arches. 5 / 10 Which branch of the ophthalmic artery passes through the supraorbital foramen? A) Central retinal artery B) Supraorbital artery C) Ethmoidal artery D) Supratrochlear artery The supraorbital artery passes through the supraorbital foramen to supply the forehead and scalp. 6 / 10 Which artery contributes to the formation of the superior palpebral arch? A) Supraorbital artery B) Medial palpebral artery C) Dorsal nasal artery D) Lacrimal artery The medial palpebral artery contributes to the superior palpebral arch along with the lateral palpebral artery. 7 / 10 Which vein provides venous drainage from the retina? A) Vorticose veins B) Superior ophthalmic vein C) Inferior ophthalmic vein D) Central retinal vein The central retinal vein provides venous drainage from the retina. 8 / 10 Which artery supplies the meninges and nasal cavity? A) Anterior ethmoidal artery B) Supratrochlear artery C) Dorsal nasal artery D) Posterior ethmoidal artery The anterior ethmoidal artery supplies the meninges and nasal cavity. 9 / 10 Which artery is the terminal branch of the ophthalmic artery? A) Central retinal artery B) Supratrochlear artery C) Dorsal nasal artery D) Supraorbital artery The dorsal nasal artery is the terminal branch of the ophthalmic artery. 10 / 10 Which branch of the ophthalmic artery pierces the sclera to supply the choroid? A) Long posterior ciliary arteries B) Lacrimal artery C) Central retinal artery D) Short posterior ciliary arteries The short posterior ciliary arteries pierce the sclera to supply the choroid. Your score is The average score is 0% Description Mnemonic for Ophthalmic Artery: DR MCLESSI D: Dorsal Nasal Artery – communicates with the angular artery of the facial artery. R: Central Retinal Artery – supplies the retina. M: Muscular branch of ophthalmic artery – supplies extraocular muscles and gives off: Anterior Ciliary Artery: Gives off a conjunctival branch for the vascular zone of the conjunctiva. Gives off a branch for the major arterial circle. C: Long and Short Posterior Ciliary Artery – pierces the eye from the back, lies in the choroid, and forms: Major Arterial Circle (MAC). Minor Arterial Circle (Intramuscular Arterial Circle – IMC). L: Lacrimal Artery – supplies the lacrimal gland. Lateral Palpebral Artery. E: Ethmoidal Artery: Anterior Ethmoidal Artery – enters the anterior cranial fossa, supplies the anterior meninges, and passes through the cribriform plate to the nasal cavity. Posterior Ethmoidal Artery. S: Supraorbital Artery – passes through the supraorbital foramen to the forehead, anastomoses with the frontal branch of the superficial temporal artery. S: Supratrochlear Artery – passes through the frontal foramen to supply the skin and muscles of the forehead. I: Internal or Medial Palpebral Artery. Ocular Circulation Major Arterial Circle of Iris (MAC): Formed by the Long Posterior Ciliary Artery and a branch of the Anterior Ciliary Artery. Supplies the iris and ciliary processes. Intramuscular Arterial Circle (IMC): Formed by the branch of the Anterior Ciliary Artery and the Short Posterior Ciliary Artery. Supplies the outer and posterior part of the ciliary muscles. Nasal Blood Supply Anterior Ethmoidal Artery. Posterior Ethmoidal Artery. Sphenopalatine Artery. Greater Palatine Artery. Superior Labial Artery. These arteries anastomose at the nasal septum, forming Little’s Area (Kisselbach’s Area), the common site of nosebleeds. Blood Supply of the Eyelids Superior Palpebral Arch and Inferior Palpebral Arch are formed by: Medial Palpebral Artery. Lateral Palpebral Artery (from Lacrimal Artery). Ophthalmic Vein Superior Ophthalmic Vein: Communicates with the angular vein as the nasofrontal vein. Central Retinal Vein drains the retina. Inferior Ophthalmic Vein: Communicates with the angular vein. Gives off a branch to the pterygoid plexus. Gives off a branch to the superior ophthalmic vein. Varicose Veins: Two superior and two inferior veins contribute to the major arterial circle and intramuscular arterial circle in the choroid. Sources Used: Memorix Anatomy (2nd Edition) – Hudák Radovan, Kachlík David, Volný Ondřej. Complete Anatomy by 3D4Medical. Biorender. University Notes and Lectures. Transcript Introduction0:03What’s up, Meditay here and In this video, we’re gonna talk detailed0:07about the vascular supply of the eyeball We’ll start with the ophthalmic artery and0:11then quickly run through the veins So – I wanna start here because0:15orientation is everything, really. If we look at the lateral view of the skull,0:19And remove the frontal and zygomatic bone We’ll be able to see the ethmoidal bone0:25And the optic canal, from which the ophthalmic artery comes from. Now I want0:29you to take a mental picture Of this specific area0:32Because I’ve simplified it in order to map the artery easier0:36So the ethmoidal bone and the optic canal is here, and for orientation sake0:41The lacrimal gland is here on the upper lateral region of each orbit0:46Now The ophthalmic artery comes through the optic0:49canal and stays on the medial side of the Eye No, for the branches,Mnemonic for
Internal Carotid Artery
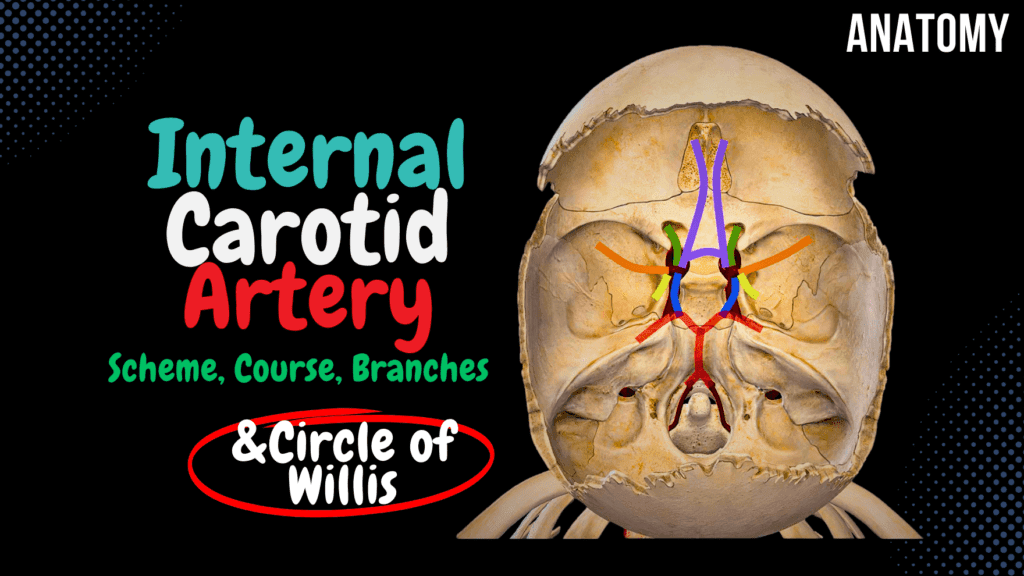
Internal Carotid Artery Scheme (Side branches, Circle of Willis) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript Notes ☆ Member Only Go to PDF Notes Illustrations ☆ Member Only Go to Illustrations 12345678910 Internal Carotid Artery – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 Which artery forms the main blood supply to the lateral surfaces of the frontal, parietal, and temporal lobes? A) Posterior cerebral artery B) Anterior cerebral artery C) Middle cerebral artery D) Ophthalmic artery The middle cerebral artery, a branch of the internal carotid artery, supplies the lateral surfaces of the brain’s hemispheres. 2 / 10 Which segment of the internal carotid artery passes through the cavernous sinus? A) Petrous segment B) Cavernous segment C) Supraclinoid segment D) Cervical segment The cavernous segment (C4) of the internal carotid artery lies within the cavernous sinus and is surrounded by cranial nerves. 3 / 10 Which segment of the internal carotid artery passes through the carotid canal? A) Cervical segment B) Cavernous segment C) Supraclinoid segment D) Petrous segment The petrous segment (C2) passes through the carotid canal, located in the temporal bone. 4 / 10 Which artery supplies the medial surface of the frontal and parietal lobes? A) Middle cerebral artery B) Anterior cerebral artery C) Anterior choroidal artery D) Posterior cerebral artery The anterior cerebral artery, a branch of the internal carotid, supplies the medial surface of the frontal and parietal lobes. 5 / 10 Which branch of the internal carotid artery supplies the retina through its central retinal branch? A) Anterior choroidal artery B) Ophthalmic artery C) Anterior cerebral artery D) Posterior communicating artery The ophthalmic artery gives rise to the central retinal artery, which supplies the retina. 6 / 10 Which clinical condition results from occlusion of the middle cerebral artery? A) Amaurosis fugax B) Contralateral hemiparesis C) Visual field defect D) Diplopia Occlusion of the middle cerebral artery can cause contralateral hemiparesis and sensory loss, often affecting the upper limb and face. 7 / 10 Which branch of the internal carotid artery participates in forming the Circle of Willis posteriorly? A) Ophthalmic artery B) Posterior communicating artery C) Anterior communicating artery D) Superior hypophyseal artery The posterior communicating artery connects the internal carotid artery to the posterior cerebral artery, forming part of the Circle of Willis. 8 / 10 Which segment of the internal carotid artery forms the carotid siphon? A) Petrous segment B) Cervical segment C) Supraclinoid segment D) Cavernous segment The cavernous segment (C4) of the internal carotid artery forms the carotid siphon. 9 / 10 Which branch of the internal carotid artery supplies the optic nerve and retina? A) Ophthalmic artery B) Posterior communicating artery C) Middle cerebral artery D) Anterior choroidal artery The ophthalmic artery, arising from the supraclinoid segment, supplies the optic nerve, retina, and orbit. 10 / 10 Which branch of the internal carotid artery contributes to the Circle of Willis? A) Posterior communicating artery B) Anterior choroidal artery C) Ophthalmic artery D) Middle cerebral artery The posterior communicating artery, a branch of the internal carotid, connects with the posterior cerebral artery. Your score is The average score is 0% Description This video covers: Parts of the Internal Carotid Canal Internal Carotid Artery and its branches: Anterior Cerebral Artery Middle Cerebral Artery Anterior Choroidal Artery Posterior Communicating Artery Blood Supply of the Brain Parts of the Internal Carotid Artery: The Internal Carotid Artery is divided into four main parts: Cervical Part Petrous Part Cavernous Part Cerebral Part Circle of Willis (Circulus Arteriosus Cerebri s. Willisi) – Thomas Willis: A critical anastomotic system at the base of the brain that ensures collateral circulation. Ophthalmic Artery Anterior Cerebral Artery Middle Cerebral Artery Anterior Choroidal Artery Posterior Communicating Artery Posterior Cerebral Artery (Branch of Basilar Artery) Cerebral Part of Internal Carotid Artery: Anterior Cerebral Artery: Runs along the longitudinal cerebral fissure. Supplies the medial surface of the frontal and parietal lobes, including: Superior Frontal Gyrus Superior Parietal Lobule Upper part of Postcentral and Precentral Gyrus Gyrus Rectus (Straight Gyrus) Middle Cerebral Artery: Clinical Note: Occlusion of this artery results in Middle Cerebral Artery Syndrome. Supplies: Insula Lentiform Nucleus Caudate Nucleus Internal Capsule Superior and Middle Temporal Gyri Large portions of the superolateral surface of the cerebral hemispheres Anterior Choroidal Artery: Runs posteriorly to form part of the choroid plexus in the lateral and third ventricles. Posterior Cerebral Artery: A branch of the basilar artery. Supplies: Occipital Lobe Inferior Temporal Gyrus Sources Used: Memorix Anatomy (2nd Edition) – Hudák Radovan, Kachlík David, Volný Ondřej. Complete Anatomy by 3D4Medical. Biorender. University Notes and Lectures. Transcript Introduction0:00alright guys so this video is about the0:02internal carotid I just want to start by0:05saying that everything you see in this0:06video was made to be schematic for you0:09to hopefully be able to visualize it now0:12essentially as the common carotid artery0:15ascends along the neck it will divide at0:17the region of the upper thyroid0:19cartilage into the external and the0:22internal carotid arteries with the0:24external carotid here in orange as we’re0:26not really going to talk about this oneParts of the Internal Carotid Artery0:28now initially the internal carotid is0:31divided into four anatomical parts0:33however in a clinical setting and this0:36really depends on the source you’re0:37studying from you may find it divided0:40into seven anatomical segments I will go0:43through the four anatomical parts but I0:45will also show you the 7-segment scheme0:48later in this video so the first part isCervical Part0:51the cervical part in the neck region0:53hence named cervical part it goes up and0:57then it goes inside the carotid canal as1:00you see here where it now becomes thePetrous Part1:03petrous part so if we take this area out1:06and visualize it a little bit you will1:09see the carotid canal here it’s1:11initially a canal within the petrous1:14part of the temporal bone so this is1:17just a coronal or a frontal section of1:20the canal now the internal carotid will1:24continue up through with the canal
External Carotid Artery
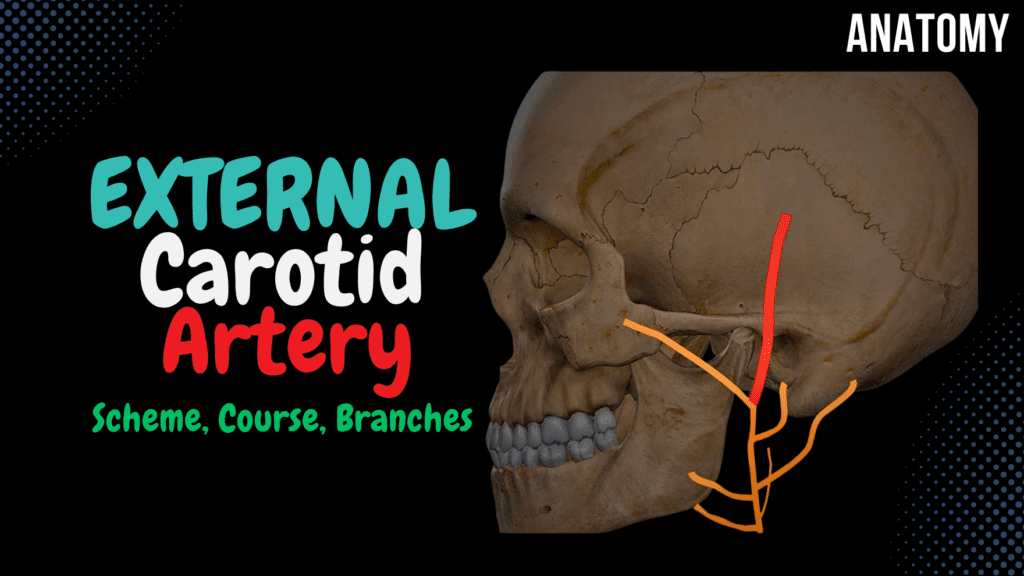
External Carotid Artery Scheme (Side branches + Mnemonics) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript Notes ☆ Member Only Go to PDF Notes Illustrations ☆ Member Only Go to Illustrations 12345678910 External Carotid Artery – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 Which branch of the facial artery supplies the chin? A) Submental artery B) Superior thyroid artery C) Ascending pharyngeal artery D) Lingual artery The submental artery, a branch of the facial artery, supplies the chin and floor of the mouth. 2 / 10 Which branch of the external carotid artery supplies the sublingual gland? A) Lingual artery B) Superior thyroid artery C) Ascending pharyngeal artery D) Facial artery The lingual artery gives rise to the sublingual artery, which supplies the sublingual gland and floor of the mouth. 3 / 10 Which artery supplies the lateral aspect of the scalp and connects with branches of the superficial temporal artery? A) Facial artery B) Occipital artery C) Ascending pharyngeal artery D) Posterior auricular artery The posterior auricular artery supplies the lateral scalp and forms anastomoses with the superficial temporal artery. 4 / 10 Which artery supplies the medial angle of the eye via its angular branch? A) Posterior auricular artery B) Facial artery C) Lingual artery D) Maxillary artery The facial artery terminates as the angular artery, supplying the medial angle of the eye. 5 / 10 Which artery gives rise to the middle meningeal artery? A) Maxillary artery B) Ascending pharyngeal artery C) Lingual artery D) Facial artery The maxillary artery gives rise to the middle meningeal artery, which supplies the dura mater of the brain. 6 / 10 Which artery supplies the posterior aspect of the auricle? A) Superficial temporal artery B) Facial artery C) Posterior auricular artery D) Occipital artery The posterior auricular artery supplies the posterior surface of the auricle and nearby scalp. 7 / 10 Which branch of the maxillary artery enters the nasal cavity to supply the septum and lateral wall? A) Inferior alveolar artery B) Sphenopalatine artery C) Lingual artery D) Facial artery The sphenopalatine artery, a terminal branch of the maxillary artery, enters the nasal cavity to supply its septum and walls. 8 / 10 Which artery supplies the dura mater through the foramen spinosum? A) Inferior alveolar artery B) Facial artery C) Middle meningeal artery D) Occipital artery The middle meningeal artery, a branch of the maxillary artery, supplies the dura mater via the foramen spinosum. 9 / 10 Which branch of the external carotid artery passes through the mandibular foramen? A) Facial artery B) Inferior alveolar artery C) Lingual artery D) Maxillary artery The inferior alveolar artery, a branch of the maxillary artery, passes through the mandibular foramen to supply the mandible and teeth. 10 / 10 Which branch of the external carotid artery supplies the posterior cranial fossa? A) Ascending pharyngeal artery B) Occipital artery C) Superior thyroid artery D) Facial artery The ascending pharyngeal artery supplies the posterior cranial fossa, pharynx, and nearby structures. Your score is The average score is 0% Description This video covers: Anatomy of the Common Carotid Artery Anatomy of the External Carotid Artery – Course and Side Branches Blood Supply of the Teeth Blood Supply of the Nasal Cavity Common Carotid Artery: Right Common Carotid Artery originates from the Aorta. Left Common Carotid Artery originates from the Brachiocephalic trunk. Ascends without side branches. Divides at the upper border of the thyroid cartilage. Contains the Carotid Body. External Carotid Artery: Mnemonic: Some Anatomists Like Freaking Out Poor Medical Students Anterior Side Branches: Superior Thyroid Artery: Muscular branches and Superior Laryngeal Artery. Lingual Artery: Deep Lingual Artery, Dorsal Lingual Artery, Sublingual Artery. Facial Artery: Mnemonic: TAGS ALL Cervical Branches of Facial Artery (TAGS): Tonsillary Artery Ascending Facial Artery Glandular Artery Submental Artery Facial Branches of Facial Artery (ALL): Angular Artery – anastomoses with Dorsal Nasal Artery. Superior and Inferior Labial Artery. Lateral Nasal Artery. Medial Side Branches: Ascending Pharyngeal Artery: Posterior Meningeal Artery, Inferior Tympanic Artery. Posterior Side Branches: Occipital Artery: Mastoid Artery and Sternocleidomastoid Artery. Posterior Auricular Artery: Auricular Branch and Stylomastoid Artery. Terminal Branches: Maxillary Artery: Temporomandibular Joint: Deep Auricular Artery. Anterior Tympanic Artery. Middle Meningeal Artery – Superior Tympanic Branch. Clinical Note: Rupture of the Middle Meningeal Artery leads to an Epidural Hematoma, causing severe headache. Inferior Alveolar Artery – Mental Branch, Dental and Peridental Branches, Mylohyoid Branch. Infratemporal Fossa: Masseteric Artery. Anterior and Posterior Deep Temporal Artery. Pterygoid Branches. Buccal Artery. Pterygopalatine Fossa: Superior Posterior Alveolar Artery. Infraorbital Artery – Superior Alveolar Artery. Descending Palatine Artery – Lesser Palatine and Greater Palatine Artery. Sphenopalatine Artery. Artery of the Pterygopalatine Canal. Superficial Temporal Artery: Frontal Branch – anastomoses with the Supraorbital Artery of the Ophthalmic Artery. Parietal Branch – anastomoses with the Posterior Auricular Artery and the Occipital Artery. Side Branches of the Temporal Artery: Anterior Auricular. Transverse Facial Artery – supplies the Parotid Gland, Masseter Muscle, and Skin. Middle Temporal Artery. Blood Supply of the Teeth: Inferior Alveolar Artery. Superior Anterior Alveolar Artery. Superior Posterior Alveolar Artery. Blood Supply of the Nasal Cavity: Greater Palatine Artery. Sphenopalatine Artery. Anterior and Posterior Ethmoidal Arteries. Superior Labial Artery. Clinical Note: These arteries form Kisselbach’s Area (Little’s Area), which is the most common site for nosebleeds when ruptured in the nasal septum. Sources Used: Memorix Anatomy (2nd Edition) – Hudák Radovan, Kachlík David, Volný Ondřej. Complete Anatomy by 3D4Medical. Biorender. University Notes and Lectures. Transcript 1. Alright so this video is going to be about the common carotid, and the external carotid artery.So before I start, I just wanna inform that the arteries and branches this video is very schematic, but hopefully they will help you get a complete picture of this topic. I’ve also put some mneumonics along the way for you to use if you want to.2. Now – we’ll start here, looking
Regulation of the Heartbeat
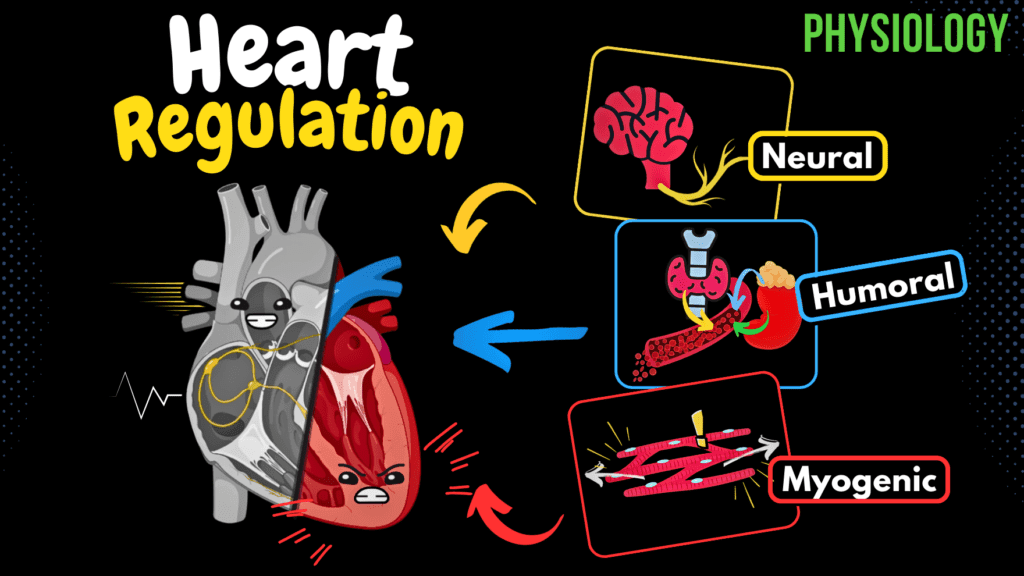
Regulation of the Heartbeat (Myogenic, Neural & Hormonal) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript 📢 Currently, there is no PDF for this video.If you’re interested in having one, feel free to send an inquiry, and I may create it in the future. BUT! There’s a quiz available in the next tab. 12345678910 Regulation of the Heartbeat – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 What happens to stroke volume during an increase in venous return? A) Increases stroke volume B) Reduces stroke volume C) Stabilizes preload D) Decreases end-diastolic volume Increased venous return raises end-diastolic volume, enhancing stroke volume via the Frank-Starling mechanism. 2 / 10 How does myogenic regulation maintain cardiac function? A) Neural input adjustments B) Changes in afterload C) Hormonal feedback D) Intrinsic stretch-based regulation Myogenic regulation involves cardiomyocytes’ intrinsic ability to autoregulate contraction strength based on stretch. 3 / 10 What mechanism reduces cardiac output at extremely high HR? A) Enhanced preload B) Increased afterload C) Decreased filling time D) Stronger ventricular contraction At very high HR, insufficient ventricular filling time decreases stroke volume and cardiac output. 4 / 10 What effect does an increase in afterload have on stroke volume? A) Decreases stroke volume B) Increases stroke volume C) Stabilizes contractility D) Enhances preload Increased afterload decreases stroke volume as the heart works harder to overcome resistance, reducing ejection. 5 / 10 What role does the renin-angiotensin-aldosterone system (RAAS) play in cardiac regulation? A) Reduces preload B) Modulates parasympathetic activity C) Increases BP and CO D) Enhances HR RAAS increases blood pressure and CO by promoting vasoconstriction and sodium/water retention. 6 / 10 What is the role of natriuretic peptides in regulating blood volume and pressure? A) Enhance afterload B) Stabilize HR C) Reduce blood volume and pressure D) Increase preload Natriuretic peptides promote sodium and water excretion, reducing blood volume and pressure. 7 / 10 What effect does acetylcholine have on the pacemaker cells of the heart? A) Enhances depolarization B) Hyperpolarizes cells C) Activates ion influx D) Increases contractility Acetylcholine hyperpolarizes pacemaker cells, reducing HR and conduction velocity. 8 / 10 What effect does the Bowditch effect (staircase effect) have on cardiac output? A) Reduces stroke volume B) Inhibits calcium influx C) Enhances contractility D) Reduces HR It enhances contractility during increased HR due to improved calcium handling in cardiomyocytes. 9 / 10 Which ion is most responsible for increasing contractility during hypercalcemia? A) Calcium B) Magnesium C) Potassium D) Sodium Calcium increases myocardial contractility and shortens the QT interval. 10 / 10 How does sympathetic stimulation affect the refractory period of cardiomyocytes? A) Inhibits calcium influx B) Shortens refractory period C) Stabilizes contraction cycle D) Prolongs refractory period Sympathetic stimulation shortens the refractory period, allowing for faster contraction rates. Your score is The average score is 0% Description Complete Cheat Code for Heart Physiology Series: 1st Video: Types of cardiac muscle, action potentials of pacemaker cells and contractile myocardium, and general properties of cardiomyocytes. 2nd Video: Detailed exploration of the cardiac cycle, including phase-by-phase events, valve operations, and pressure differences. 3rd Video: Cardiac output. 4th Video: Regulation of heartbeat. Key Concepts Covered: 1. Overview of Cardiac Output (CO): Formula: CO = Heart Rate (HR) × Stroke Volume (SV). Regulation affects pacemaker activity or myocardial contraction. 2. Regulation Categories: Myogenic Regulation: Heterometric Regulation: Frank-Starling Mechanism: Increased end-diastolic volume (EDV) stretches cardiomyocytes, enhancing contraction and increasing SV. Homeometric Regulation: Bowditch Effect (Staircase Effect): Increased HR strengthens contractions due to enhanced calcium handling in cells. Neural Regulation: Involves the nervous system, divided into extracardiac and intracardiac regulation. Extracardiac Regulation: Sympathetic Nervous System: Increases HR, contractility, and CO via norepinephrine and epinephrine acting on β1-adrenergic receptors. Activates ion channels to enhance calcium influx, increasing contraction strength and speed. Parasympathetic Nervous System: Reduces HR and conduction velocity via acetylcholine on muscarinic receptors. Inhibits adenylyl cyclase, decreasing cAMP levels and activating K+ channels to hyperpolarize the membrane. Medullary Control: Integrates input from baroreceptors and chemoreceptors to modulate autonomic nervous system activity. Intracardiac Regulation: Intramural ganglia modulate cardiac function independent of direct CNS control. Humoral Regulation: Involves hormones in the blood influencing HR, contractility, and CO. Epinephrine: Released by adrenal medulla, activating β1-adrenergic receptors. Renin-Angiotensin-Aldosterone System (RAAS): Angiotensin II increases contractility, vasoconstriction, and blood volume. Aldosterone promotes sodium and water reabsorption, increasing blood pressure and CO. Thyroid Hormones (T3): Increase HR and contractility by influencing gene expression and ion channel activity. Glucocorticoids: Enhance myocardial contractility and adrenergic receptor sensitivity. Natriuretic Peptides (ANP, BNP): Reduce blood volume and pressure by promoting sodium and water excretion. 3. Ion Regulation: Calcium: Hypercalcemia increases contractility, shortening the QT interval. Hypocalcemia decreases contractility, prolonging the QT interval. Potassium: Hyperkalemia depolarizes cells, increasing arrhythmia risk. Hypokalemia reduces excitability, making depolarization more difficult. By understanding these regulatory mechanisms, you’ll gain a comprehensive understanding of how the body maintains cardiac function under various physiological conditions. #cardiacphysiology #heartfunction #extracardiac #ecg #medicaleducation #usmlepreparation #nursingeducation #premed #heartanatomy Sources: University lectures and notes Barrett, K. E., Barman, S. M., Boitano, S., & Brooks, H. L. (2016). Ganong’s Review of Medical Physiology (25th ed.). McGraw-Hill Education. Hall, J. E. (2016). Guyton and Hall Textbook of Medical Physiology (13th ed.). Elsevier. Mohrman, D. E., & Heller, L. J. (2014). Cardiovascular Physiology (11th ed.). McGraw-Hill Education. Biorender Transcript Introduction0:06Regulation of the Heartbeat Physiology What’s up, Taim talks med here. Let’s continue our Complete Cheat Code for Heart Physiology.0:13We’re doing this in 4 segments. The 1st video was about the different types of cardiac muscle, the action potentials of pace maker cells and contractile myocardium,0:22and the general properties of our cardiomyocytes. The 2nd video was about the cardiac cycle where we0:28made an easy diagram illustrating what actually happens at each phase. The 3rd video covered0:33everything you need to know regarding the cardiac output. This is the 4th video where we’ll cover the regulation of the
Cardiac Output
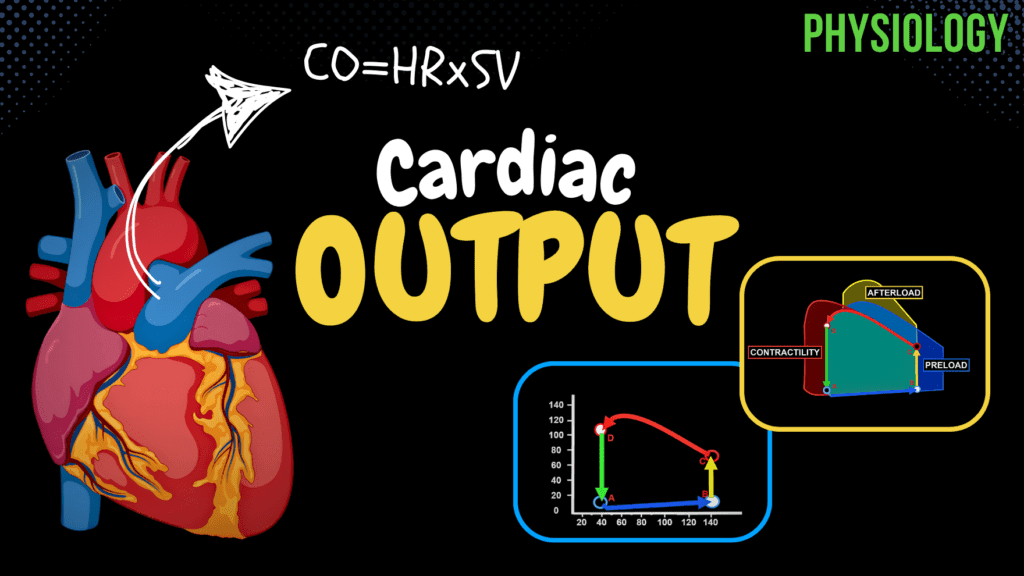
Cardiac Output (Preload, Afterload, Pressure-Volume Diagram) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript 📢 Currently, there is no PDF for this video.If you’re interested in having one, feel free to send an inquiry, and I may create it in the future. BUT! There’s a quiz available in the next tab. 12345678910 Cardiac Output – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 What is the maximum pressure-volume relationship? A) Constant pressure B) Relationship between pressure and volume C) No relationship D) Sudden increase in pressure The pressure-volume relationship shows the heart’s response to end-diastolic volume and systolic pressure. 2 / 10 What does the ejection fraction measure? A) Amount of blood remaining in ventricles B) Percentage of blood ejected C) Resistance during contraction D) Maximum stroke volume Ejection fraction measures the percentage of blood ejected from the ventricle relative to end-diastolic volume. 3 / 10 What is the approximate stroke volume in a resting adult? A) 100-150 ml B) 50-100 ml C) 30-50 ml D) 10-30 ml Stroke volume is about 50-100 ml per beat. 4 / 10 What is the relationship between stroke volume and cardiac output? A) Independent of heart rate B) Inversely proportional to afterload C) Directly proportional to heart rate D) Directly proportional to cardiac output Stroke volume multiplied by heart rate determines cardiac output. 5 / 10 How does heart rate influence cardiac output at very high rates (>150 bpm)? A) Increases cardiac output B) Has no effect C) Decreases cardiac output D) Causes arrhythmias Cardiac output decreases at very high heart rates due to insufficient ventricular filling. 6 / 10 What is the physiological significance of the pressure-volume loop? A) Assess heart function B) Predict arrhythmias C) Measure blood oxygenation D) Analyze electrical activity Pressure-volume loops help evaluate heart function and valve health. 7 / 10 What is the normal cardiac output at rest? A) 10-12 liters B) 2-3 liters C) 5-7 liters D) 15-20 liters Normal cardiac output at rest is 5-7 liters per minute. 8 / 10 How does contractility affect cardiac output? A) Lowers cardiac reserve B) Reduces ventricular filling C) Enhances cardiac output D) Stabilizes blood pressure Increased contractility leads to stronger ventricular contractions, enhancing cardiac output. 9 / 10 What is the term for the amount of blood in the ventricles before contraction? A) Stroke volume B) Preload C) Contractility D) Afterload Preload refers to the volume of blood in the ventricles before contraction. 10 / 10 What is the approximate cardiac output at rest in a healthy adult? A) 8-10 liters B) 5-7 liters C) 2-3 liters D) 12-15 liters Cardiac output at rest is about 5-7 liters per minute. Your score is The average score is 0% Description Complete Cheat Code for Heart Physiology: 1st Video: Types of cardiac muscle, action potentials of pacemaker cells and contractile myocardium, and general properties of cardiomyocytes. 2nd Video: Detailed exploration of the cardiac cycle, including phase-by-phase events, valve operations, and pressure differences. 3rd Video: Cardiac output. 4th Video: Regulation of heartbeat. What is Cardiac Output? Definition: The amount of blood ejected from each ventricle per minute. Formula: Cardiac Output = Heart Rate (bpm) × Stroke Volume (L/beat) Units: Measured in liters per minute (L/min). Visualizing Cardiac Output Heart Anatomy: Right and left atria, ventricles, aorta. Cardiac Cycle Phases: Atrial systole Isovolumetric contraction Ejection phase (systolic phase) Isovolumetric relaxation Passive filling phase (common diastolic phase) Stroke Volume: Amount of blood ejected per beat (~50-100 ml). Heart Rate: Number of beats per minute. Factors Determining Cardiac Output Heart Rate: Increased HR typically increases cardiac output, but >150 bpm may reduce it due to inadequate ventricular filling. Stroke Volume: Depends on: Venous Return: More blood entering the heart leads to greater output. Contractility: Stronger contractions eject more blood. Aortic Resistance: Higher resistance (hypertension, plaque) reduces stroke volume. Normal Cardiac Output At Rest: ~5-7 L/min During Exercise: ~15-30 L/min Pressure-Volume Relationship Diastolic Phase: Ventricular filling, gradual pressure increase. Systolic Phase: Ventricular contraction, pressure rises then falls. Isovolumetric Phases: Contraction and relaxation phases with no volume change. Clinical Relevance Pressure-Volume Curves: Assess heart function, muscle efficiency, and valve health. Abnormal PV Loops: Right Shift: Increased preload (more blood in, more ejected). Increased Afterload: Higher aortic pressure, harder for the heart to eject blood. Increased Contractility: Stronger contractions, more blood ejected. Factors Affecting Cardiac Output Preload: Volume of blood before contraction. Afterload: Resistance ventricles overcome to eject blood. Contractility: Strength of ventricular contraction. Regulation of Heartbeat Mechanisms: Myogenic, neural, and humoral regulation. Conclusion Summary: Discussed cardiac output, pressure-volume curve, and effects of preload, afterload, and contractility. Next Video: Regulation of heartbeat. #cardiacphysiology #heartfunction #cardiacoutput #ecg #medicaleducation #usmlepreparation #nursingeducation #premed #heartanatomy Sources: University lectures and notes Barrett, K. E., Barman, S. M., Boitano, S., & Brooks, H. L. (2016). Ganong’s Review of Medical Physiology (25th ed.). McGraw-Hill Education. Hall, J. E. (2016). Guyton and Hall Textbook of Medical Physiology (13th ed.). Elsevier. Mohrman, D. E., & Heller, L. J. (2014). Cardiovascular Physiology (11th ed.). McGraw-Hill Education. Biorender Transcript Introduction0:08What’s up, Taim talks med here. Let’s continue our Complete Cheat Code for Heart Physiology.0:13We’re doing this in 4 segments. The 1st video was about the different types of cardiac muscle,0:18the action potentials of pace maker cells and contractile myocardium, and the general0:22properties of our cardiomyocytes. In the 2nd video we looked detailed into the cardiac cycle. In this0:28video we’re gonna cover everything you need to know regarding the cardiac output. And in0:33the next video we’ll cover the regulation of the Heartbeat, covering all the most0:38important mechanisms that actually change the contractility and heart rate. Alright awesome.What is Cardiac Output?0:44Now how do we define cardiac output? Cardiac output is the mount of blood that is ejected0:50from each ventricle during one contraction. Let’s visualize this. Here’s the heart. We got0:56the right and the left atria, the right and the left ventricles, and
Cardiac Cycle
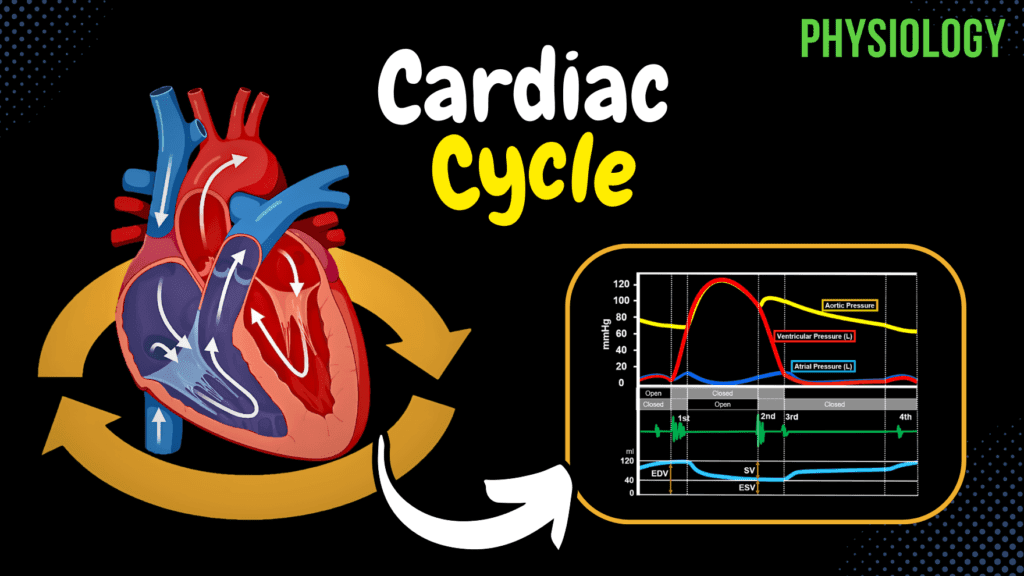
Cardiac Cycle (Pressure-Graph) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript 📢 Currently, there is no PDF for this video.If you’re interested in having one, feel free to send an inquiry, and I may create it in the future. BUT! There’s a quiz available in the next tab. 12345678910 Cardiac Cycle – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 What does the cardiac cycle refer to? A) Pressure differences in the heart B) Valve mechanics C) Electrical conduction of the heart D) Mechanical events of one heartbeat The cardiac cycle includes the phases of contraction and relaxation during one heartbeat. 2 / 10 What does stroke volume (SV) depend on? A) EDV and ESV B) Ventricular relaxation C) Blood oxygen content D) Atrial pressure SV depends on end-diastolic volume, end-systolic volume, and myocardial contractility. 3 / 10 Which heart sound is most commonly absent in healthy adults? A) S3 B) S1 C) S4 D) S2 S4 is typically absent in healthy adults and indicates strong atrial contraction when present. 4 / 10 Which phase of the cardiac cycle involves no change in blood volume but increased pressure? A) Ventricular ejection B) Isovolumetric contraction C) Passive filling D) Atrial systole Isovolumetric contraction involves increased ventricular pressure without a change in volume. 5 / 10 What is the normal range for the ejection fraction (EF)? A) 40-50% B) 20-40% C) 60-80% D) 50-70% The normal EF range is 50-70%, indicating the percentage of EDV ejected during systole. 6 / 10 What is the primary cause of the second heart sound (S2)? A) Semilunar valve closure B) Blood exiting atria C) AV valve closure D) Blood entering ventricles S2 is caused by the closure of semilunar valves at the start of diastole. 7 / 10 Which phase of the cardiac cycle involves atrial contraction? A) Isovolumetric contraction B) Ventricular ejection C) Atrial systole D) Passive filling Atrial systole is the phase where both atria contract to push blood into the ventricles. 8 / 10 What heart sound is heard during the closure of AV valves? A) S2 B) S3 C) S1 D) S4 The first heart sound (S1) occurs during AV valve closure at the start of ventricular systole. 9 / 10 Which phase is characterized by the AV valves opening and blood entering the ventricles? A) Passive filling B) Isovolumetric contraction C) Atrial systole D) Isovolumetric relaxation Passive filling is characterized by AV valve opening and blood flow into the ventricles. 10 / 10 Which heart sound corresponds to semilunar valve closure? A) S4 B) S3 C) S1 D) S2 The second heart sound (S2) is heard during the closure of the semilunar valves. Your score is The average score is 0% Description Complete Cheat Code for Heart Physiology Series: 1st Video: Types of cardiac muscle, action potentials of pacemaker cells and contractile myocardium, and general properties of cardiomyocytes. 2nd Video: Detailed exploration of the cardiac cycle, including phase-by-phase events, valve operations, and pressure differences. 3rd Video: Cardiac output. 4th Video: Regulation of heartbeat. Phases of the Cardiac Cycle: The cardiac cycle consists of mechanical events in one heartbeat, including contraction (systole) and relaxation (diastole). Atrial Systole (0.1s): Atria contract, pushing blood into ventricles. Isovolumetric Contraction (0.04s): Ventricles contract, but valves remain closed. Ventricular Ejection (0.26s): Ventricles push blood into the aorta and pulmonary artery. Isovolumetric Relaxation (0.08s): Ventricles relax, no blood flow into ventricles. Passive Filling (0.32s): AV valves open, ventricles fill passively. Valve Operations and Pressure Differences: Bottle Cap Phenomenon: Demonstrates how pressure controls valve function. Pressure Curve and Graphical Representation: Vertical Axis: Blood pressure (mmHg). Horizontal Axis: Time (seconds). Red: Left ventricular pressure. Blue: Left atrial pressure. Yellow: Aortic pressure. Heart Sounds: S1 (First Heart Sound): Closure of AV valves, start of systole. S2 (Second Heart Sound): Closure of semilunar valves, start of diastole. S3 (Third Heart Sound): Passive ventricular filling. S4 (Fourth Heart Sound): Strong atrial contraction. Ventricular Volumes: End Diastolic Volume (EDV): 110-150 ml. Stroke Volume (SV): 60-100 ml. Reserve Volume: 20-40 ml. Residual Volume: Volume never ejected. Ejection Fraction (EF): Normal 50-70%, reduced in heart failure. #cardiacphysiology #heartfunction #cardiaccycle #ecg #medicaleducation #usmlepreparation #nursingeducation #premed #heartanatomy Sources: University lectures and notes. Barrett, K. E., Barman, S. M., Boitano, S., & Brooks, H. L. (2016). Ganong’s Review of Medical Physiology (25th ed.). McGraw-Hill Education. Hall, J. E. (2016). Guyton and Hall Textbook of Medical Physiology (13th ed.). Elsevier. Mohrman, D. E., & Heller, L. J. (2014). Cardiovascular Physiology (11th ed.). McGraw-Hill Education. Biorender. Transcript Introduction0:08What s up, Taim talks med here. Let s continue our Complete Cheat Code for Heart Physiology.0:13We re doing this in 4 segments. The 1st video was about the different types of cardiac muscle,0:18the action potentials of pace maker cells and contractile myocardium, and the general0:22properties of our cardiomyocytes. In this video we will look detailed into the cardiac cycle,0:28and draw a curve and understand what happens at each phase. In the 3rd video we ll cover0:33everything you need to know regarding the cardiac output. And in the 4th video where we ll cover0:38the regulation of the Heartbeat, covering all the most important mechanisms that actually change the0:43contractility and heart rate. Alright awesome. Cardiac cycle is basically just the beginningWhat is Cardiac Cycle?0:50of one heartbeat to the beginning of the next. And it includes all the mechanical0:55events happening within one heartbeat. So If you look here, this is the heart,1:00and here it s pumping continuously. Showing you one cardiac cycle after the other,1:05and if we remove the walls as it s pumping, you ll see that there are specific events happening.1:11And if you just stare at this heart, focus on one chamber, you ll notice that one cardiac1:17cycle consists of two periods: one during which the heart muscle relaxes and refills with blood,1:23called diastole, following a period of contraction and pumping of blood, called systole.1:29What we
Cardiac Muscle
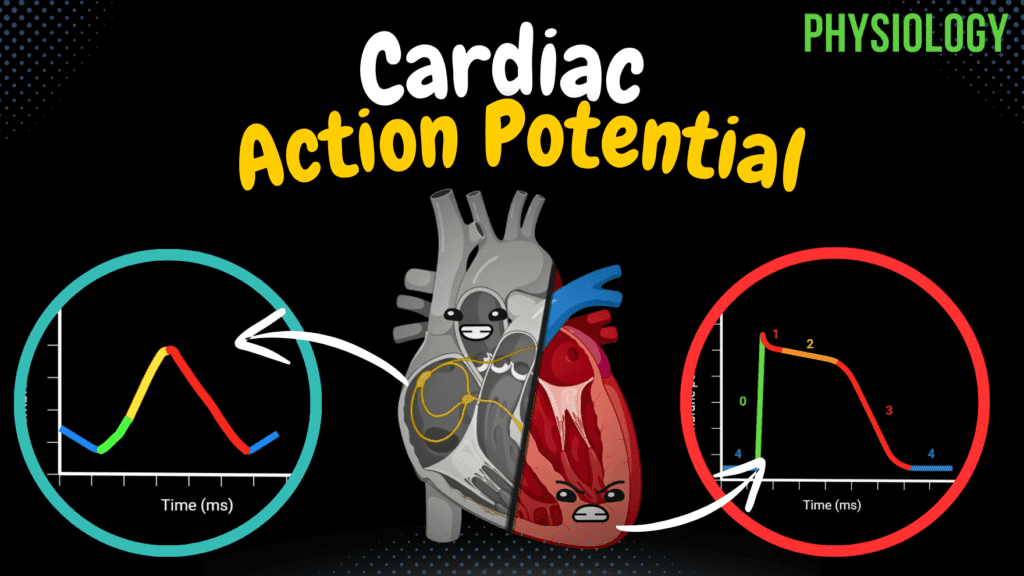
Cardiac Muscle (Action Potential, Automaticity, ARP, RRP) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript 📢 Currently, there is no PDF for this video.If you’re interested in having one, feel free to send an inquiry, and I may create it in the future. BUT! There’s a quiz available in the next tab. 12345678910 Cardiac Muscle – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 What is the function of atrial natriuretic peptide (ANP)? A) Increases heart rate B) Stimulates vasoconstriction C) Promotes vasodilation D) Contracts the myocardium ANP promotes vasodilation and reduces sodium and water reabsorption in the kidneys to regulate blood volume. 2 / 10 What is the stable resting membrane potential of contractile cells? A) -60 mV B) -85 mV C) 0 mV D) -90 mV Contractile cells have a stable resting membrane potential of approximately -85 mV. 3 / 10 What is the primary pacemaker of the heart? A) SA node B) Purkinje fibers C) AV node D) Bundle of His The sinoatrial (SA) node is the primary pacemaker of the heart, setting the rhythm at 60-80 beats per minute. 4 / 10 What is the primary function of pacemaker cells in the heart? A) Promote vasodilation B) Secrete hormones C) Generate and propagate electrical impulses D) Contract the myocardium Pacemaker cells generate and propagate electrical impulses due to their automaticity. 5 / 10 Which ion is responsible for the rapid depolarization (Phase 0) of contractile cells? A) Cl- B) Ca2+ C) Na+ D) K+ Na+ influx through voltage-gated sodium channels causes rapid depolarization in contractile cells. 6 / 10 What structure sets the primary rhythm of the heart? A) Bundle of His B) SA node C) AV node D) Purkinje fibers The sinoatrial (SA) node is the heart’s primary pacemaker. 7 / 10 What is the primary location of contractile cardiomyocytes? A) Endocardium B) SA node C) Myocardium D) Epicardium Contractile cardiomyocytes are located in the myocardium. 8 / 10 Why does the AV node delay conduction of electrical impulses? A) To speed up conduction B) To stabilize action potentials C) To synchronize heart sounds D) To allow atrial contraction The AV node slows conduction (0.1 m/s) to ensure atrial contraction before ventricular contraction. 9 / 10 What ion influx is critical during the plateau phase of contractile cells? A) K+ B) Ca2+ C) Cl- D) Na+ Ca2+ influx through L-type channels is critical during the plateau phase. 10 / 10 Which layer of the heart generates the contraction force? A) Epicardium B) Endocardium C) Pericardium D) Myocardium The myocardium is responsible for generating the heart’s contractile force. Your score is The average score is 0% Description Complete Cheat Code for Heart Physiology Series: 1st Video: Types of cardiac muscle, action potentials of pacemaker cells and contractile myocardium, and general properties of cardiomyocytes. 2nd Video: Detailed exploration of the cardiac cycle, including phase-by-phase events, valve operations, and pressure differences. 3rd Video: Cardiac output. 4th Video: Regulation of heartbeat. Types of Cardiac Muscle Cells: 1. Pacemaker Cells (Nodal Cells): Location: SA node, AV node, Bundle of His, RBB, LBB, Purkinje fibers. Function: Generate and propagate electrical impulses. Action Potential: No stable resting membrane potential. “Funny” Na+ channels allow slow Na+ influx, triggering depolarization. T-type and L-type Ca2+ channels open, causing a rapid influx of Ca2+. Repolarization occurs via K+ efflux. 2. Contractile Cells: Location: Myocardium. Function: Generate the force of contraction. Action Potential: Stable resting membrane potential (-85 mV). Depolarization via Na+ influx, plateau phase due to Ca2+ influx balanced by K+ efflux, followed by repolarization. 3. Endocrine Cells: Location: Atria and ventricles. Function: Secrete ANP and BNP to regulate blood pressure and fluid balance. Conduction System of the Heart: SA Node: Primary pacemaker (60-80 BPM). AV Node: Secondary pacemaker (40-60 BPM), slows conduction. Bundle of His and Purkinje Fibers: Rapidly conduct impulses through ventricles. Action Potentials: A Comparative View Pacemaker Cells: Phase 4: Slow depolarization via “funny” Na+ channels. Phase 0: Rapid depolarization via Ca2+ influx. Phase 3: Repolarization via K+ efflux. Contractile Cells: Phase 0: Rapid depolarization via Na+ influx. Phase 1: Initial repolarization via K+ efflux. Phase 2: Plateau phase via Ca2+ influx. Phase 3: Repolarization via K+ efflux. Phase 4: Resting membrane potential. Electrical Conduction Pathway: Impulse generation at SA Node. Atrial conduction (1 m/s). AV Node delay (0.1 m/s) ensures proper atrial emptying. Ventricular conduction via Purkinje fibers (1-4 m/s). Refractory Periods: Absolute Refractory Period (ARP): No response to stimuli. Relative Refractory Period (RRP): Strong stimulus may trigger an action potential. Effective Refractory Period (ERP): Combination of ARP and early RRP. Properties of Cardiomyocytes: Automaticity All-or-none law Long refractory periods Sources: University lectures and notes Barrett, K. E., Barman, S. M., Boitano, S., & Brooks, H. L. (2016). Ganong’s Review of Medical Physiology (25th ed.). McGraw-Hill Education. Hall, J. E. (2016). Guyton and Hall Textbook of Medical Physiology (13th ed.). Elsevier. Mohrman, D. E., & Heller, L. J. (2014). Cardiovascular Physiology (11th ed.). McGraw-Hill Education. Biorender Transcript Introduction0:08What s up, Taim talks med here. I ve now simplified all the most important high yield topics in heart physiology, so this is the Complete Cheat Code0:18We re doing this in 4 segments. This is the 1st video where we re going talk detailed about the different types of cardiac muscle, the action potentials of pace maker cells and contractile0:27myocardium, and the general properties of our cardiomyocytes. The 2nd video will be about the cardiac cycle. The 3rd video we ll cover everything you need to know regarding the0:36cardiac output. And in the 4th video we ll cover the regulation of the Heartbeat, covering all the0:42most important mechanisms that actually change the contractility and heart rate. Alright awesome.You should already know0:48Alright, so I m starting this video assuming that you have some pre knowledge in the anatomy of the0:54heart. I m basically assuming that you already know
Anatomy of the Heart – Layers & Conducting System
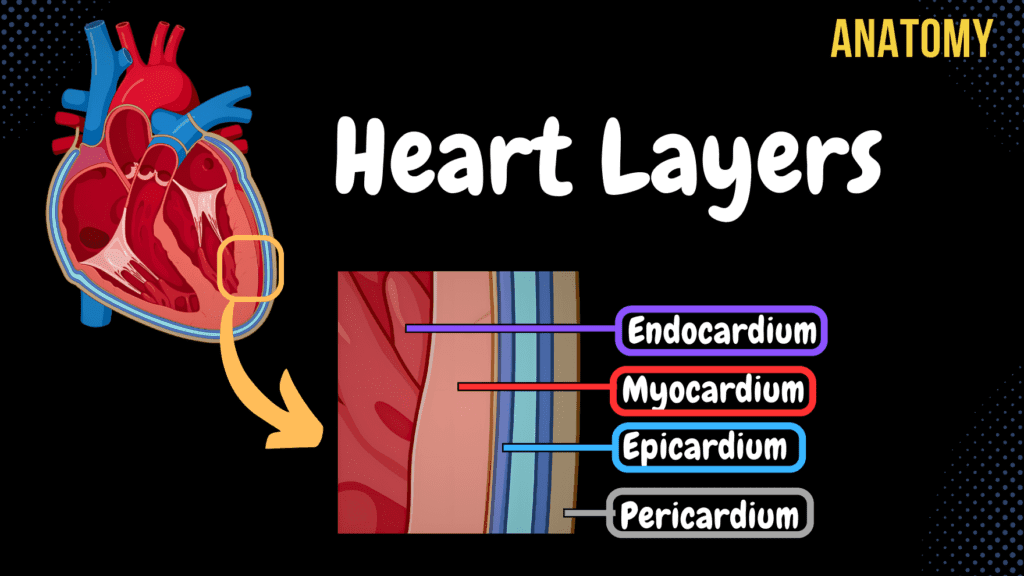
Anatomy of the Heart – Layers, Conducting System & Topography Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript Notes ☆ Member Only Go to PDF Notes Illustrations ☆ Member Only Go to Illustrations 12345678910 Heart Anatomy (Layers) – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 What structure lies laterally to the heart according to its syntopy? A) Esophagus B) Great blood vessels C) Diaphragm D) Pleura The pleura lies laterally to the heart according to its syntopy. 2 / 10 Which structure is located at the medial wall of the right atrium? A) Valve of coronary sinus B) Crista terminalis C) Fossa ovalis D) Interatrial septum The interatrial septum is located at the medial wall of the right atrium. 3 / 10 Which part of the myocardium contains longitudinal muscle fibers? A) Endocardial layer B) Epicardial layer C) Superficial and deep layers D) Middle layer The superficial and deep layers of the myocardium contain longitudinal muscle fibers. 4 / 10 Where is the mitral valve auscultated? A) Fifth intercostal space, right of sternum B) Fifth intercostal space, midclavicular line C) Fourth intercostal space, left of sternum D) Second intercostal space, right of sternum The mitral valve is auscultated at the fifth intercostal space at the midclavicular line. 5 / 10 What is the innermost layer of the heart? A) Endocardium B) Pericardium C) Epicardium D) Myocardium The endocardium is the innermost layer of the heart. 6 / 10 What is the visceral lamina of the serous pericardium also called? A) Parietal lamina B) Epicardium C) Myocardium D) Endocardium The visceral lamina of the serous pericardium is also called the epicardium. 7 / 10 What is the function of the fibrous pericardium? A) Aids in atrial contraction B) Facilitates electrical conduction C) Provides structural support D) Produces heart sounds The fibrous pericardium provides structural support and protects the heart. 8 / 10 Which pericardial sinus is located posterior to the ascending aorta and pulmonary trunk? A) Aortic sinus B) Transverse pericardial sinus C) Fibrous pericardial sinus D) Oblique pericardial sinus The transverse pericardial sinus is located posterior to the ascending aorta and pulmonary trunk. 9 / 10 What structure connects the myocardium and epicardium? A) Serous pericardium B) Fibrous pericardium C) Endocardium D) Chordae tendineae The serous pericardium connects the myocardium and the epicardium. 10 / 10 Which pericardial layer allows frictionless movement of the heart? A) Myocardium B) Fibrous pericardium C) Endocardium D) Serous pericardium The serous pericardium, with its visceral and parietal layers, allows frictionless movement of the heart. Your score is The average score is 0% Description This video covers the layers of the heart, its conducting system, and topography, including its holotopy, skeletopy, and syntopy. Understanding these aspects is crucial for medical students and professionals studying cardiovascular anatomy. Layers of the Heart: Serous Pericardium Fibrous Pericardium Endocardium Myocardium Epicardium Endocardium: Forms the cusps of the following valves: Bicuspid Valve Tricuspid Valve Aortic Valve Pulmonary Valve Valve of the Inferior Vena Cava (Vulva Vena Cava Inferioris) Valve for the Coronary Sinus (Vulva Sinus Coronarii) Myocardium: Forms fibrous rings and muscle layers: Myocardium of the Atria: Superficial Circular Muscle Fibers Deep Longitudinal Muscle Fibers Form Pectinate Muscle (Musculi Pectinati) Myocardium of the Ventricles: Deep Layer: Longitudinal Muscle Fibers Middle Layer: Circular Muscle Fibers Superficial Layer: Longitudinal Muscle Fibers Deep and Superficial layers form the Vortex of the Heart (Vortex Cordis) Left ventricle is thicker than the right ventricle Forms Trabeculae Carneae and Papillary Muscles (Musculi Papillares) Epicardium: It is the visceral lamina of the serous pericardium. Pericardium: Serous Pericardium (Pericardium Serosum) Visceral Lamina (Epicardium) Parietal Lamina Fibrous Pericardium (Pericardium Fibrosum) Pericardial Cavity (Cavitas Pericardiaca) Transverse Pericardial Sinus (Sinus Transversus Pericardii) Oblique Pericardial Sinus (Sinus Obliquus Pericardii) Conducting System of the Heart: Sinoatrial Node (SA Node) Atrioventricular Node (AV Node) Bundle of His Left Bundle Branch Right Bundle Branch Purkinje Fibers Topography of the Heart: Holotopy of the Heart: The heart lies in the mediastinum medium Skeletopy of the Heart: Superior Border: 3rd rib horizontally Right Border: Parallel to sternal margin (Linea Parasternalis) Lower Border: From the cartilage of the 5th rib to the 5th intercostal space Left Border: 5th intercostal space to the level of the 4th rib Openings of the Heart: Atrioventricular Openings: From the 3rd rib to the 6th sternal junction Aortic and Pulmonary Openings: From the 3rd sternal junction to the 4th sternal junction Topography of the Valves of the Heart: Aortic and Pulmonary Valve: Located at the 2nd intercostal space Tricuspid and Bicuspid (Mitral) Valve: Located at the 5th intercostal space Syntopy of the Heart: Anteriorly: Behind the sternum Posteriorly: Esophagus Laterally: Pleura Inferiorly: Diaphragm Superiorly: Great blood vessels Sources Used in This Video: Memorix Anatomy 2nd Edition by Hudák Radovan, Kachlík David, Volný Ondřej Biorender University Notes and Lectures Transcript Introduction0:03What’s up.0:04Meditay here.0:05Let’s talk about the heart again.0:07In the last video, we covered the circulation system and the general anatomy of the heart.0:12Now In this video, We’re going to cover the Layers of the heart, which include the Endocardium,0:16Myocardium, and Epicardium.0:19Then we’ll go through the conducting system.0:21And after that, we’re going to look at the general topography of the heart, which will0:25help you from a clinical perspective.0:27Let’s go through all of these starting with the layers of the heart.Layers of the Heart0:31So here you see a raw picture of the heart without any type of coverings.0:35In real life, the heart is covered by a wet surface called serous pericardium.0:40And then by another layer of dense connective tissue called fibrous pericardium.0:44We’ll now start by cut the heart like this, so see all the layers.0:48Then we’ll take a small segment, and zoom in.0:52Now we’re able to see all the layers of the heart, which include the endocardium,0:56myocardium and the Epicardium.0:59These three layers are what is considered a part of the actual heart.1:02The Serous and Fibrous pericardium we saw
Anatomy of the Heart – External & Internal Structures
Anatomy of the Heart – External & Internal Structures Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript Notes ☆ Member Only Go to PDF Notes Illustrations ☆ Member Only Go to Illustrations 12345678910 Heart Anatomy (Structures) – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 What is the main function of the papillary muscles? A) Conduct electrical impulses B) Pump blood into the atria C) Open the heart valves D) Prevent valve prolapse Papillary muscles contract to tighten chordae tendineae, preventing valve prolapse during ventricular contraction. 2 / 10 Which groove is associated with the anterior interventricular branch? A) Posterior interventricular sulcus B) Coronary sulcus C) Sulcus terminalis D) Anterior interventricular sulcus The anterior interventricular sulcus contains the anterior interventricular artery and great cardiac vein. 3 / 10 Which structure carries impulses from the atrioventricular node to the ventricles? A) Internodal pathways B) SA node C) Bundle of His D) Purkinje fibers The Bundle of His transmits impulses from the AV node to the bundle branches, ensuring ventricular contraction. 4 / 10 What is the function of the nodules in the semilunar valves? A) Allow backflow of blood B) Assist chordae tendineae C) Facilitate blood ejection D) Ensure valve closure The nodules ensure complete closure of the semilunar valves by sealing the cusps. 5 / 10 What is the function of the chordae tendineae? A) Open the semilunar valves B) Facilitate atrial contraction C) Conduct electrical impulses D) Prevent valve prolapse The chordae tendineae anchor the atrioventricular valve cusps to papillary muscles, preventing valve prolapse. 6 / 10 Which arteries arise from the left coronary artery? A) Right coronary artery B) Circumflex and anterior interventricular C) Left marginal and diagonal arteries D) Posterior interventricular artery The left coronary artery gives rise to the circumflex artery and anterior interventricular artery. 7 / 10 What is the primary function of the pulmonary valve? A) Prevents ventricular inversion B) Prevents backflow into the ventricle C) Directs blood to coronary arteries D) Supplies oxygenated blood The pulmonary valve prevents backflow of blood into the right ventricle from the pulmonary trunk. 8 / 10 What is the function of the left auricle? A) Facilitates blood oxygenation B) Pumps blood into ventricles C) Increases atrial capacity D) Prevents valve regurgitation The left auricle increases the capacity of the left atrium and assists in blood collection. 9 / 10 What is the name of the opening between the right atrium and right ventricle? A) Pulmonary trunk B) Ostium of coronary sinus C) Right atrioventricular opening D) Left atrioventricular opening The right atrioventricular opening allows blood to flow from the right atrium to the right ventricle. 10 / 10 Which structure separates the right and left ventricles internally? A) Interatrial septum B) Crista terminalis C) Sulcus terminalis D) Interventricular septum The interventricular septum divides the right and left ventricles and consists of muscular and membranous parts. Your score is The average score is 0% Description This video covers the blood circulation in the body and the anatomy of the heart, including its external and internal structures. Understanding the pathway of blood through the heart and its anatomical components is essential for mastering cardiovascular physiology and anatomy. Blood Circulation in the Body: Pulmonary Circulation (Circulus Sanguid Minor): Deoxygenated blood enters the right atrium through the superior and inferior vena cava. Blood flows through the tricuspid valve into the right ventricle. The right ventricle pumps blood through the pulmonary valve into the pulmonary artery. The pulmonary artery carries blood to the lungs for oxygenation. Systemic Circulation (Circulus Sanguis Major): Oxygenated blood returns from the lungs into the left atrium. The left atrium sends blood through the bicuspid (mitral) valve into the left ventricle. The left ventricle pumps blood through the aortic valve into the aorta. The aorta distributes oxygenated blood throughout the body. External Structures of the Heart: Apex of the Heart (Apex Cordis) Base of the Heart (Basis Cordis) Pulmonary Surface (Facies Pulmonalis) Sternocostal Surface (Facies Sternocostalis) Diaphragmatic Surface (Facies Diaphragmatica) Right Border / Right Margin of the Heart (Margo Dexter Cordis) Coronary Sulcus (Sulcus Coronarius) Anterior Interventricular Sulcus (Sulcus Interventricularis Anterior) Posterior Interventricular Sulcus (Sulcus Interventriculare Posterior) Internal Structures of the Heart: Septum of the Heart (Septum Cordis): Interventricular Septum (Septum Interventriculare) Muscular Part (Pars Muscularis) Membranous Part (Pars Membranacea) Interatrial Septum (Septum Interatriale) Right Atrium: Anterior Wall: Right Auricle (Auricula Dextra) Superior Wall: Opening of Superior Vena Cava (Ostium Vena Cava Superioris) Posterior Wall: Opening of Inferior Vena Cava (Ostium Vena Cava Inferiores) Sinus of Vena Cava (Sinus Venarum) Terminal Crest (Crista Terminalis) Medial Wall: Interatrial Septum, Oval Fossa (Fossa Ovalis) Inferior Wall: Right Atrioventricular Opening (Ostium Atrioventriculare Dextrum), Tricuspid Valve Right Ventricle: Trabeculae Carneae Papillary Muscles (Musculi Papillares) Tricuspid Valve (Anterior, Posterior, and Septal Cusps) Pulmonary Valve Left Atrium: Anterior Wall: Left Auricle (Auricula Sinister) Posterior Wall: Pulmonary Veins and Openings of Pulmonary Veins (Ostia Venarum Pulmonalium) Medial Wall: Interatrial Septum Left Ventricle: Bicuspid (Mitral) Valve (Anterior, Posterior, and Commissural Cusps) Aortic Valve (Vulva Aortae) Trabeculae Carneae Papillary Muscles and Tendinous Chords Sources Used in This Video: Memorix Anatomy 2nd Edition by Hudák Radovan, Kachlík David, Volný Ondřej Complete Anatomy by 3D4Medical Biorender University Notes and Lectures Transcript Introduction0:03Hey, What’s up. Meditay here. Let’s talk about the anatomy of the heart. In this video,0:08We’re first going to look at how the blood circulates in the body.0:11After that, we’re going to cover the different external structures you’ll find on the surface0:16of the heart. Then we’re going to open up the heart and go through the internal structures of0:20each chamber, which include the right and left atrium and the right and left ventricles.0:25Then in the next video, we’ll talk about the layers of the heart’s wall,0:29the conducting system, and then the topography. Now, let’s start with the circulation.Blood Circulation System0:33So here is see the anterior view of the thorax, right?0:37If you
