Complement System
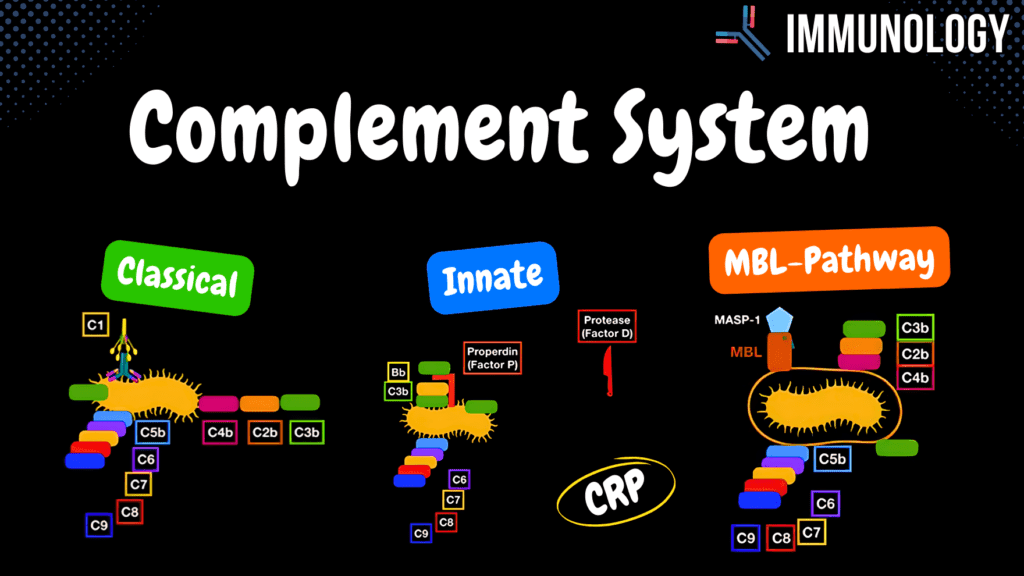
Complement System Pathways (Classical, Alternative, MBL) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript 📢 Currently, there is no PDF for this video.If you’re interested in having one, feel free to send an inquiry, and I may create it in the future. BUT! There’s a quiz available in the next tab. 12345678910 Complement System – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 Which cytokine is responsible for acute phase protein production in the liver during infection? A) IL-6 B) TNFα C) IL-1 D) IL-8 IL-6 induces the production of acute phase proteins like CRP and MBL in the liver. 2 / 10 What triggers the Mannose Binding Lectin pathway of complement activation? A) MBL binding to mannose B) Antibodies binding C) C3 spontaneous cleavage D) Acute phase proteins Mannose Binding Lectin binds to mannose residues on the surface of pathogens like fungi. 3 / 10 Which complement factor amplifies the classical pathway by forming a feedback loop? A) C4a B) C3b C) C5a D) Properdin C3b amplifies the classical pathway by enhancing the formation of C5 convertase. 4 / 10 What is the function of the C3 convertase enzyme in the complement system? A) Cleaves C3 B) Activates cytokines C) Neutralizes toxins D) Forms MAC C3 convertase cleaves C3 into C3a and C3b, initiating further amplification of the complement cascade. 5 / 10 What is the main trigger for the lectin pathway of complement activation? A) Antibodies B) C3 spontaneous cleavage C) MBL binding D) Cytokine release Binding of Mannose Binding Lectin (MBL) to mannose residues on pathogens activates the lectin pathway. 6 / 10 Which complement pathway does not lead to the formation of a Membrane Attack Complex (MAC) on capsules? A) Classical Pathway B) Mannose Binding Lectin Pathway C) Lectin Pathway D) Alternative Pathway The Mannose Binding Lectin pathway does not form a MAC on capsules, as it targets exposed mannose residues. 7 / 10 What is the role of C1q in the classical pathway of complement activation? A) Binds antibodies B) Activates cytokines C) Forms C5 convertase D) Cleaves C4 C1q binds to the Fc region of antibodies attached to pathogens, initiating the classical pathway. 8 / 10 What is the significance of MASP-1 in the Mannose Binding Lectin pathway? A) Stabilizes C3 convertase B) Activates cytokines C) Acts as a serine protease D) Forms MAC MASP-1 binds to MBL and acts as a serine protease to cleave complement proteins. 9 / 10 What is the role of anaphylatoxins like C3a, C4a, and C5a in the immune response? A) Promotes antigen presentation B) Increase vascular permeability C) Neutralizes antigens D) Forms Membrane Attack Complex Anaphylatoxins increase capillary permeability and activate mast cells, contributing to inflammation. 10 / 10 What is the role of C3a in the complement cascade? A) Neutralizes antigens B) Forms C5 convertase C) Anaphylatoxin D) Activates MAC C3a acts as an anaphylatoxin, promoting inflammation by increasing vascular permeability and activating mast cells. Your score is The average score is 0% Description This video is part 3 of Innate Immunity – Complement System (Humoral Factors). All information in my immunology videos is sourced from: Book: Immunology, Eighth Edition by David Male, Jonathan Brostoff, David Roth, and Ivan Roitt Additional research: PubMed University lecture materials Mechanisms of the Complement System: Membrane Attack Complex (MAC) Chemotaxis Opsonization Anaphylatoxins Classical Pathway: Antibody-dependent (Adaptive Immune System) Step 1: C1q binds to antibody-antigen complex Step 2: C1r activates C1s Step 3: C1s cleaves C4 and C2 Step 4: C4b and C2b form C3 convertase Step 5: C3 convertase cleaves C3, which binds to the surface as an opsonin or binds to C3 convertase to form C5 convertase Step 6: Membrane Attack Complex (MAC) forms on Gram-negative bacteria Alternative Pathway: Antibody-independent Step 1: C3 undergoes spontaneous cleavage in the bloodstream. C3b binds to bacterial surfaces Step 2: Factor B binds Step 3: Factor D cleaves Factor B into Bb Step 4: Properdin (Factor P) stabilizes the complex, forming C3 convertase Step 5: The pathway proceeds as in the classical pathway Mannose-Binding Lectin (MBL) Pathway: Triggered by Acute Phase Response Step 1: Active macrophages release IL-1, IL-6, and TNF-α as endogenous pyrogens Step 2: Cytokines travel to the hypothalamus, triggering Prostaglandin E2 (PGE2) release and causing fever Step 3: IL-6 signals the liver to release acute phase proteins, including C-reactive protein (CRP) and Mannose-Binding Lectin (MBL) C-Reactive Protein (CRP) Functions: Acts as an opsonin Activates the classical pathway of the complement system Mannose-Binding Lectin (MBL) Pathway: Activation begins 1-2 days after infection Step 1: MBL binds to Mannose (monosaccharide) on fungal capsules and surfaces Step 2: MBL recruits MASP-1 (Mannan-binding Lectin Serine Protease 1), which functions as an enzyme Step 3: The pathway proceeds as in the classical pathway Note: The Membrane Attack Complex (MAC) does not form on capsules. Complement System Effector Functions: C4a, C5a, and C3a: Act as Anaphylatoxins by increasing capillary permeability and activating mast cells Function in Chemotaxis by directing phagocytes to infection sites Complement system removes immune complexes from the bloodstream Transcript Introduction0:00the compliment system is a part of the0:02immune system that enhances the defense0:04against pathogens and there are0:06different mechanisms that the complement0:08system actually has that allows it to0:10help the immune system one of these ways0:13is that it forms this complex on the0:15surface of the micro organisms called0:17the membrane attack complex which makes0:19holes on the membrane of the micro0:21organisms and these holes going to0:23disturb the environment inside the cell0:26by water leaking in causing cell lysis0:29so what more can I do you know when a0:32macrophage is just circling around your0:33body the complement system acts as0:36something called chemotaxis where they0:38go tell the macrophage hey I found a0:40bacteria can come and kill it hence I0:42underlined the word taxi because it0:44actually works at a taxi for the0:45macrophages it tells them where to go0:47all the things we can do is work as0:49obstinate and optimize
Innate Immune System
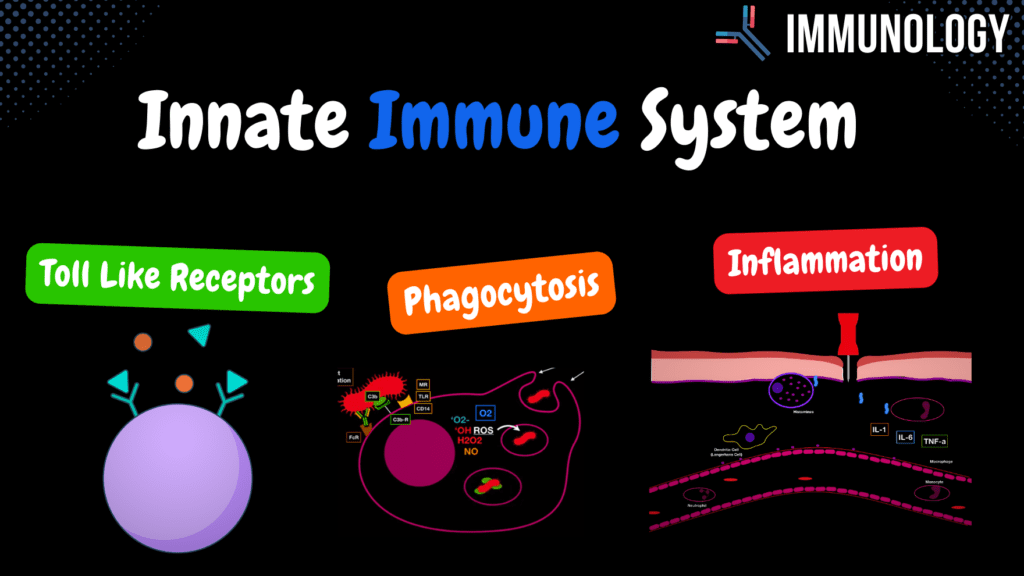
Innate Immune System (Toll Like Receptors, Phagocytosis & inflammation ) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript 📢 Currently, there is no PDF for this video.If you’re interested in having one, feel free to send an inquiry, and I may create it in the future. BUT! There’s a quiz available in the next tab. 12345678910 Innate Immune System (Inflammation) – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 What is the role of TNFα during inflammation? A) Neutralizes toxins B) Activates NK cells C) Enhances phagocytosis D) Activates endothelial cells TNFα activates endothelial cells and contributes to vascular permeability. 2 / 10 Which Toll-Like Receptor (TLR) recognizes unmethylated CpG islands in bacterial DNA? A) TLR3 B) TLR7 C) TLR9 D) TLR4 TLR9 recognizes unmethylated CpG DNA, which is common in bacterial genomes. 3 / 10 Which Toll-Like Receptor (TLR) is involved in recognizing bacterial lipopolysaccharides (LPS)? A) TLR4 B) TLR1 C) TLR3 D) TLR5 TLR4 recognizes LPS, a component of gram-negative bacterial cell walls. 4 / 10 Which Toll-Like Receptor (TLR) recognizes single-stranded viral RNA? A) TLR3 B) TLR9 C) TLR5 D) TLR7 TLR7 recognizes single-stranded RNA from viruses, triggering an antiviral response. 5 / 10 Which step in phagocytosis involves the fusion of a phagosome with a lysosome? A) Formation of phagolysosome B) Binding C) Engulfment D) Antigen presentation The fusion of a phagosome with a lysosome leads to the formation of a phagolysosome for pathogen digestion. 6 / 10 What is the role of reactive oxygen species (ROS) in phagocytosis? A) Bind to PAMPs B) Neutralize toxins C) Activate complement D) Kill pathogens ROS mediate oxygen-dependent killing of engulfed pathogens. 7 / 10 Which cells are classified as professional phagocytes? A) Neutrophils B) B cells C) Plasma cells D) NK cells Neutrophils, macrophages, dendritic cells, and mast cells are professional phagocytes. 8 / 10 What is the role of opsonization in phagocytosis? A) Activate complement system B) Secrete cytokines C) Enhance pathogen binding D) Neutralize toxins Opsonization enhances pathogen binding by marking them for phagocytosis with antibodies or complement proteins. 9 / 10 What is the role of macrophages in antigen presentation? A) Secrete complement B) Neutralize toxins C) Present antigens to T cells D) Produce antibodies Macrophages present antigens to T cells using MHC class I or II molecules. 10 / 10 What is the role of lysosomes in phagocytosis? A) Digest pathogens B) Release cytokines C) Bind pathogens D) Present antigens Lysosomes release enzymes for oxygen-independent digestion of pathogens. Your score is The average score is 0% Description This video is part 2 of Innate Immunity – Cellular Factors (Toll-like Receptors, Phagocytosis, and Inflammation). All information in my immunology videos is sourced from: Book: Immunology, Eighth Edition by David Male, Jonathan Brostoff, David Roth, and Ivan Roitt Additional research: PubMed University lecture materials TLR dimerization: Link Toll-like Receptors (TLRs): Location: Epithelial Cells of the mucous membrane Endothelial Cells Macrophages Dendritic Cells Neutrophils Membrane-bound TLRs: TLR 1/2 and TLR 2/6: Recognize Peptidoglycan/Lipoteichoic acid, Lipoproteins TLR 4: Recognizes Lipopolysaccharides, Fungal Mannan, Viral Envelope Proteins TLR 5: Recognizes Bacterial Flagellin Intracellular Receptors: TLR 3: Recognizes Double-stranded RNA from viruses TLR 7: Recognizes Single-stranded RNA TLR 8: Recognizes Double-stranded RNA from viruses TLR 9: Recognizes Unmethylated CpG islands Toll-like Receptors trigger: Release of cytokines (TNF, IL-1, IL-12) Release of chemokines (IL-8) Release of antiviral cytokines (IFN α/β) Phagocytosis: Professional Phagocytes: Neutrophils Macrophages/Monocytes Mast Cells Dendritic Cells Steps in Phagocytosis: Binding: Non-specific surface receptors (Mannose Receptor, Toll-like Receptor, CD14), Indirect Opsonization (C3b), Direct Opsonization (Fc receptor to antibody) Engulfment: Pseudopods wrap around the bacteria Phagosome Formation: Enclosure of the pathogen within a vesicle Digestion: Oxygen-dependent digestion (Reactive Oxygen Species) Oxygen-independent digestion Lysosome: Breaks down bacterial cell walls Enzymes: Proteolytic and hydrolytic enzymes Antimicrobial peptides (Defensins) Acidic reactions (low pH) Lactoferrin (in neutrophils) Antigen Presentation: Presented on MHC class I or II, or released into interstitial fluid to be absorbed by lymph vessels Macrophage Cytokine Release: Interleukin 8: Chemotaxis for Leukocytes Interleukin 1: Activates T-Lymphocytes and Macrophages Interleukin 6: Activates T- and B-Lymphocytes TNF-α: Activates Endothelium Interleukin 12: Activates Natural Killer Cells Endogenic Pyrogens (Fever Induction): IL-1, IL-6, TNF-α stimulate the hypothalamus to release Prostaglandins E2 IL-6 stimulates the liver to release acute phase proteins Incomplete Phagocytosis: Some bacteria evade digestion: Listeria: Releases Listeriolysin to escape phagosomes Mycobacterium tuberculosis: Produces catalase to resist degradation Immune System in Inflammation: Swelling: Due to increased permeability of blood vessels Pain: Due to diapedesis and edema pressing on pain receptors Heat: Due to increased blood flow Redness: Caused by vasodilation Transcript Introduction 0:00 and the last video we looked at the 0:01 general factors in the innate immune 0:03 system now we’re going to look at the 0:05 cellular factors in the immune system 0:07 which generally includes the taluk 0:09 receptors the phagocytosis and 0:10 inflammation natural killer cells and 0:13 the microbiota also a part of the 0:15 cellular factors keep that in mind so 0:18 we’ll start with Tullock receptors Toll-Like Receptors 0:20 toddler preceptors are receptors you 0:22 don’t really hear about so much but 0:25 they’re actually a really important part 0:27 of the body’s nonspecific resistance and 0:29 they’re really good at activating both 0:31 innate and adaptive immunity you will 0:34 find these receptors on specific areas 0:36 in your body you will find them lining 0:38 the epithelial cells of the mucous 0:40 membranes at portland’s of entry this 0:43 includes the MCOs of the nasal cavity 0:44 the mouth esophagus lungs and many more 0:47 you will also find them lining in detail 0:50 yourselves of the blood vessels this is 0:52 very very crucial because it helps the 0:54 body detect microorganisms very fast and 0:57 you won’t just find them on tissue 0:58 you’ll also find them in cells of the 1:01 first line of defense like
Innate Immune System Overview
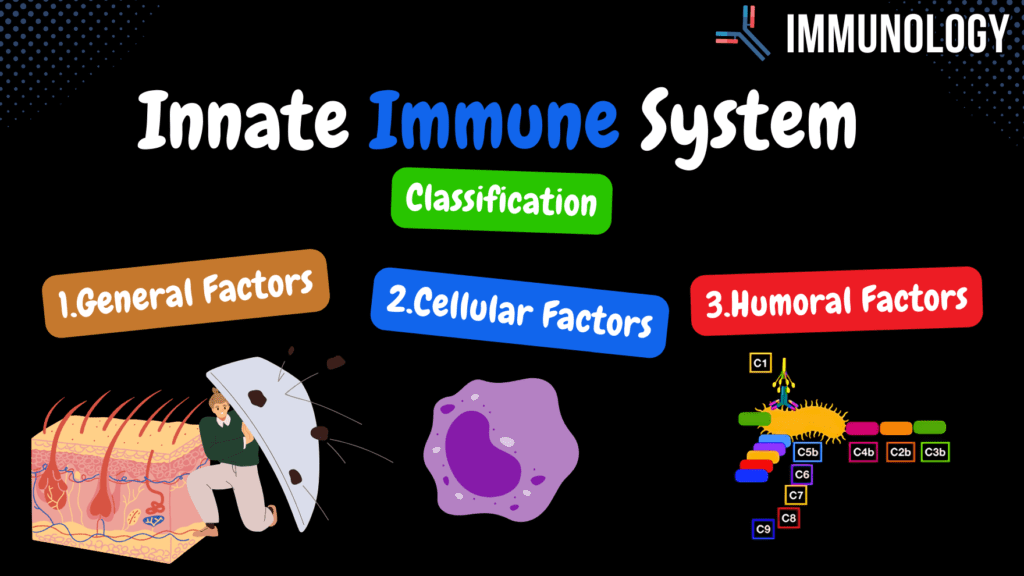
Innate Immune System: Simple Overview (Classification, General Factors) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript 📢 Currently, there is no PDF for this video.If you’re interested in having one, feel free to send an inquiry, and I may create it in the future. BUT! There’s a quiz available in the next tab. 12345678910 Innate Immune System Overview – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 What is the purpose of the complement system in innate immunity? A) Decreases inflammation B) Stimulates fever C) Enhances phagocytosis D) Activates NK cells The complement system enhances phagocytosis, promotes inflammation, and directly lyses pathogens. 2 / 10 Which cellular factor in innate immunity destroys pathogens via engulfment? A) NK cells B) TLRs C) Phagocytes D) Complement proteins Phagocytes, like macrophages, engulf and destroy pathogens. 3 / 10 What innate immune process directly lyses pathogens? A) Toll-like receptors B) Complement system C) NK cells D) Defensins The complement system lyses pathogens by forming membrane attack complexes. 4 / 10 What role do natural killer cells play in innate immunity? A) Destroy infected cells B) Neutralize toxins C) Activate PAMPs D) Secrete lysozyme NK cells identify and destroy infected or abnormal cells without prior activation. 5 / 10 What substance secreted by mucous membranes destroys bacterial cell walls? A) Interferons B) Lysozyme C) Defensins D) Pepsin Lysozyme, secreted by mucous membranes, destroys bacterial cell walls to protect against infection. 6 / 10 What do defensins secreted by mucous membranes do? A) Stimulate inflammation B) Disrupt pathogen membranes C) Neutralize toxins D) Activate complement Defensins are antimicrobial peptides that disrupt the membranes of pathogens. 7 / 10 What distinguishes innate immunity from acquired immunity? A) Specific, gains memory B) Non-specific, no memory C) Non-specific, gains memory D) Specific, no memory Innate immunity is non-specific and lacks immunological memory, attacking all agents equally. 8 / 10 Which general factor of innate immunity is influenced by pyrogenic reactions? A) Complement system B) Skin C) Fever D) Phagocytosis Pyrogenic reactions like fever are general factors that help fight infections by raising body temperature. 9 / 10 Which innate immune component detects and binds PAMPs? A) Lysozyme B) NK cells C) Complement proteins D) Toll-like receptors Toll-like receptors (TLRs) detect and bind pathogen-associated molecular patterns (PAMPs). 10 / 10 Which innate immune component directly attacks viral infections? A) Interferons B) Complement system C) Lysozyme D) Phagocytosis Interferons are proteins that interfere with viral replication and activate immune responses. Your score is The average score is 0% Description This video is part 1 of Innate Immunity – Classification and General Factors. All information in my immunology videos is sourced from: Book: Immunology, Eighth Edition by David Male, Jonathan Brostoff, David Roth, and Ivan Roitt Additional research: PubMed University lecture materials Difference between Innate and Acquired Immunity: Innate Immunity: Non-specific No immunological memory Attacks all agents equally Acquired Immunity: Specific defense Gains immunological memory Classification of Innate Immunity: General Factors: Barriers (Skin and Gastrointestinal tract) Pyrogenic reactions (Fever) Secretion Cellular Factors: Microbiota Phagocytosis Natural Killer Cells Toll-like Receptors Inflammatory reaction Humoral Factors: Complement System Interferons General Factors: Skin: Physical barrier due to tight junctions Secretion of antimicrobial products Mucous Membranes: Contain antimicrobial substances such as lysozyme, pepsin, and defensins Low pH provides additional protection Transcript Introduction0:00hello and welcome to another video this0:02video is mainly going to be about the0:03innate immune system now your immune0:06system uses two main strategies to0:08defeat any type of unwanted invaders one0:11of the strategies is called the innate0:12immune system and the other ones called0:14acquired immune system the innate immune0:16system is mainly present since birth and0:18is therefore sometimes also called the0:20natural immune system0:21well they acquired however forms during0:23a person’s lifetime and is therefore0:25sometimes also called the adapted now0:27just remember that the baby also has0:30some type of acquired immune system I0:31just put the baby there to show you that0:33you’ve always had the innate immune0:35system ever since you were born so now0:37let’s put this to practice imagine we0:39have three different types of bacteria0:40right the innate immune system is what0:43we call nonspecific because it actually0:46works against any type of agents equally0:48the adaptive however works very specific0:52as you see right here and not only that0:55upon defeating the bacteria you gain0:57some kind of immunological memory which0:59usually becomes enhanced upon repeated1:02exposure to the same agents the innate1:05immunity doesn’t really have that as1:06well let’s see how that works we mainlyClassification of the Innate Immune System1:09classify the immune system into three1:11different types the first is well called1:13general factors and we’ve got the1:15cellular factors and also have the1:17humoral factors the general factors1:20include physiological barriers at the1:23portal of entry like the skin and the1:25mucous membranes and they’re usually1:28analogically enough the first line of1:30defense next we have the para genetic1:33reactions now don’t get scared if you1:34haven’t heard this term before I’ll get1:36more into this later on talk about the1:38macrophages mainly but pyrogenic1:41reactions often refer to as fever some1:45viruses and bacterias cannot really1:47replicate optimally because the body1:49changes its temperature so that’s why we1:52call it the general factors because it1:55works generally by increasing the1:56temperature another general factors are2:00secretion inab secretion of different2:02enzymes fatty acids the cellular factors2:05we got your own microbiota fighting for2:07space and food the phagocytosis by cells2:11like neutrophils and macrophages2:13they do that by the different receptors2:16they have in the surface I also got2:18natural killer cells so they’re really2:19important for the antiviral immune2:21response these cells can bind to surface2:25of antigens by using toll-like receptors2:27which usually to inflammatory response2:30you also get humoral factors which2:32include the complement system at the2:34interference now I know this seems a lot2:36but trust me it all gets logical once2:39you understand the concept in my opinion2:41if you want to learn immunology properly2:43you need to understand different parts2:46individually before you can understand2:49the whole concept together in in system2:51and that’s what I’m aiming to show you2:54everything individually first and then2:56put them all together and show you have2:58this wort in the system alright so inGeneral
Peritoneum
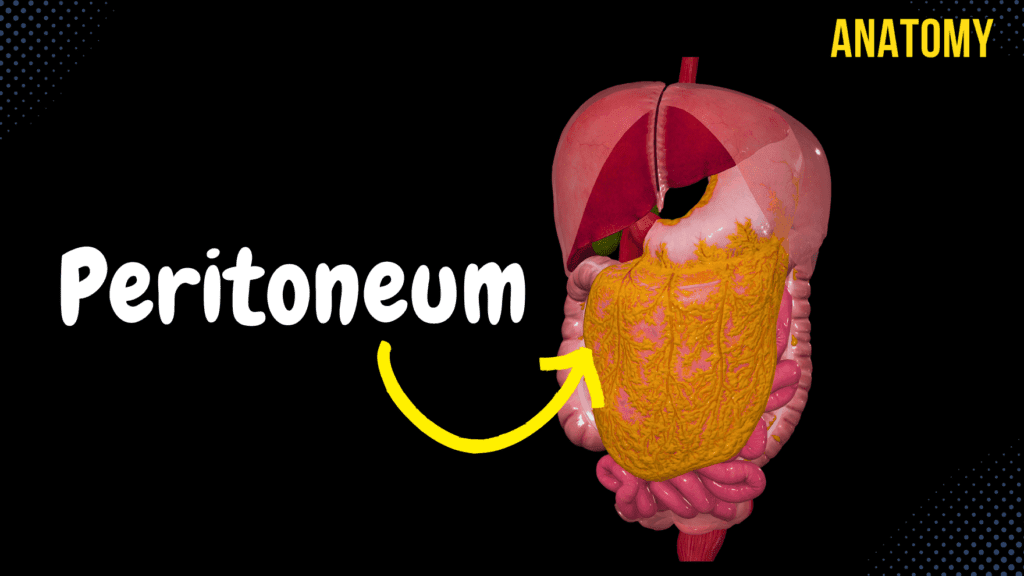
Peritoneum (Parts, Lesser & Greater Omentum, Mesentery, Peritoneal Cavity) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript Notes ☆ Members Only Go to PDF Notes Illustrations ☆ Members Only Go to Illustrations 12345678910 Peritoneum – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 What is the clinical significance of the omental (epiploic) foramen? A) Site of Ligament Attachment B) Pathway for Arteries C) Communication Between Sacs D) Junction of Viscera The omental foramen allows communication between the greater and lesser sacs of the peritoneal cavity. 2 / 10 What type of fluid is contained within the peritoneal cavity? A) Pancreatic Juice B) Bile C) Mucus D) Serous Fluid Serous fluid lubricates the peritoneal cavity to reduce friction between organs. 3 / 10 Which level of the peritoneal cavity contains the omental bursa? A) Lower Level B) Middle Level C) Entire Peritoneal Cavity D) Upper Level The omental bursa is located in the upper level of the peritoneal cavity. 4 / 10 What is the role of the root of the mesentery? A) Separate Peritoneal Levels B) Anchor Intestines to Wall C) Aid in Digestion D) Produce Lymph The root of the mesentery anchors the small intestine to the posterior abdominal wall and allows passage for vessels. 5 / 10 What is the anatomical term for the peritoneal cavity pouch between the uterus and rectum in females? A) Rectouterine Pouch B) Retrocecal Pouch C) Vesicouterine Pouch D) Rectovesical Pouch The rectouterine pouch (pouch of Douglas) lies between the uterus and rectum. 6 / 10 What is the peritoneal attachment for the small intestine? A) Mesentery B) Greater Omentum C) Lesser Omentum D) Retroperitoneum The mesentery provides attachment for the small intestine. 7 / 10 Which part of the peritoneum lines the abdominal wall? A) Mesentery B) Parietal Peritoneum C) Visceral Peritoneum D) Greater Omentum The parietal peritoneum lines the abdominal and pelvic walls. 8 / 10 What is the primary function of the omental bursa? A) Separate Lobes B) Reduce Friction and Facilitate Movement C) Support Vessels D) Absorb Nutrients The omental bursa reduces friction and facilitates organ movement. 9 / 10 What is the primary lymphatic drainage of the peritoneal cavity? A) Paracolic Nodes B) Hepatic Nodes C) Mesenteric Lymph Nodes D) Splenic Nodes The mesenteric lymph nodes provide drainage for the peritoneal cavity. 10 / 10 What structure connects the liver to the anterior abdominal wall? A) Gastrophrenic Ligament B) Coronary Ligament C) Falciform Ligament D) Hepatoduodenal Ligament The falciform ligament connects the liver to the anterior abdominal wall. Your score is The average score is 0% Description This video is about the anatomy of the peritoneum. Parts of the Peritoneum: Parietal Peritoneum (peritoneum parietale) – Lines the internal surface of the abdominal and pelvic wall. Visceral Peritoneum (peritoneum viscerale) – Covers the walls of organs. Peritoneal Cavity (cavitas peritonealis) – The space between the parietal and visceral peritoneum. Visceral Peritoneum: How does the Visceral Peritoneum Cover the Organs? Intraperitoneal Viscera: Organs completely covered by the peritoneum. Mesoperitoneal Viscera: Partly covered by the peritoneum (on three different sides). Retroperitoneal Viscera: Covered by the peritoneum only on one side. The Course of the Peritoneum: Parietal peritoneum continues into the visceral peritoneum through: Falciform Ligament (ligamentum falciforme hepatis) Coronary Ligament (ligamentum coronarium hepatis) Right Triangular Ligament (ligamentum triangulare dextrum) Left Triangular Ligament (ligamentum triangulare sinistrum) These ligaments cover the liver. Lesser Omentum: Consists of all ligaments under the liver but above the lesser curvature of the stomach. Lesser Omentum: Hepatogastric Ligament (ligamentum hepatogastricum) Hepatoduodenal Ligament (ligamentum hepatoduodenale) Both start at the porta hepatis of the liver. Greater Omentum: Gastrophrenic Ligament (ligamentum gastrophrenicum) Gastrosplenic Ligament (ligamentum gastrosplenicum) Gastrocolic Ligament (ligamentum gastrocolicum) Course: Extends downward in front of the abdominal organs until reaching the terminal line of the pelvis (linea terminalis), then turns around and attaches to the omental tenia (tenia omentalis) on the transverse colon. Ends at the mesocolic tenia (tenia mesocolica) and transitions into the transverse mesocolon (mesocolon transversum). Mesentery: Transverse Mesocolon (mesocolon transversum) Root of Mesentery (radix mesenterii) Mesentery completely encloses the intestines, provides structural support, and forms pathways for blood vessels. Peritoneal Cavity (Cavitas Peritonealis): The peritoneal cavity is divided into three levels: Upper Level (above the transverse mesocolon) Middle Level (below the transverse mesocolon but above the terminal line of the pelvis) Lower Level (in the lesser pelvis) Upper Level: Contains 2 recesses and 1 bursa. Recess: A small opening. Bursa: A fluid-filled sac. Structures in the upper level: Subphrenic Recess (recessus subphrenicus) Subhepatic Recess (recessus subhepaticus) Omental Bursa (bursa omentalis) Walls/Borders of the Omental Bursa: The Omental Bursa contains the Omental Foramen/Epiploic Foramen (foramen omentale/foramen epiploicum), bordered by the Vestibule of the Omental Bursa (vestibulum bursa omentalis). Recesses of the Bursa Omentalis: Superior Recess (recessus superior) Inferior Recess (recessus inferior) Splenic Recess (recessus splenicus) Middle Level of the Peritoneal Cavity: Superior Duodenal Recess (recessus duodenalis superior) Inferior Duodenal Recess (recessus duodenalis inferior) Superior Ileocecal Recess (recessus ileocaecalis superior) Inferior Ileocecal Recess (recessus ileocaecalis inferior) Retrocecal Recess (recessus retrocaecalis) Intersigmoid Recess (recessus intersigmoideus) Lower Level of the Peritoneal Cavity: In this level, the term excavatio means a pouch. Female: Rectouterine Pouch (excavatio rectouterina) Vesicouterine Pouch (excavatio vesicouterina) Male: Rectovesical Pouch (excavatio rectovesicalis) Sources: Memorix Anatomy 2nd Edition by Hudák Radovan, Kachlík David, Volný Ondřej Biorender University Notes and Lectures Transcript Introduction0:03What’s up. Meditay here. And in this video, we’re gonna go through the anatomy of the peritoneum,0:08which is the serous membrane that lines the inside of the abdominal wall,0:12as well as surrounding various organs we have inside the abdominal cavity.0:17So in this video, we’ll first cover the parts of the peritoneum.0:21Then we’ll go through the lesser and greater omentum and the mesentery.0:25After that, we’ll look at the different structures you’ll find in the peritoneal cavity.0:30So now, now that we’ve covered the anatomy of the organs in the abdominal cavity,0:35We need something
Bile Pathway, Gall Bladder & Pancreas
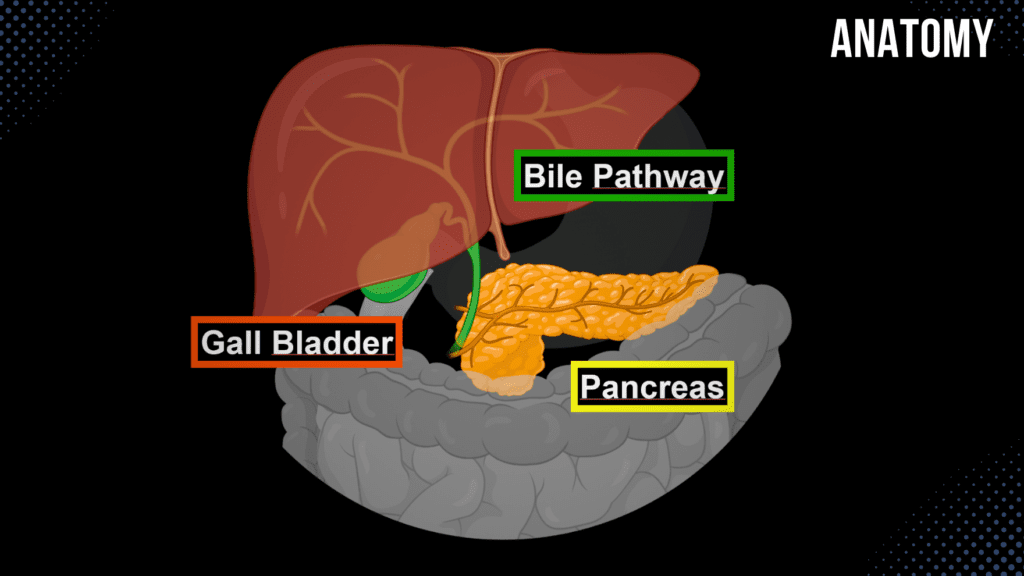
Bile Pathway, Gall Bladder & Pancreas Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript Notes ☆ Member Only Go to PDF Notes Illustrations ☆ Member Only Go to Illustrations 12345678910 Bile and Pancreas – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 What is the primary function of the pancreatic islets (Islets of Langerhans)? A) Hormone Secretion B) Emulsify Lipids C) Secrete Digestive Enzymes D) Neutralize Acid The islets secrete hormones such as insulin and glucagon for blood sugar regulation. 2 / 10 What separates the uncinate process from the body of the pancreas? A) Superior Mesenteric Vessels B) Hepatic Vein C) Splenic Artery D) Inferior Vena Cava The superior mesenteric vessels pass between the uncinate process and the body of the pancreas. 3 / 10 Which duct carries bile from the liver to the gallbladder? A) Cystic Duct B) Hepatic Duct C) Common Bile Duct D) Pancreatic Duct The cystic duct carries bile to the gallbladder for storage. 4 / 10 Which artery primarily supplies the body and tail of the pancreas? A) Inferior Mesenteric Artery B) Splenic Artery C) Celiac Trunk D) Superior Mesenteric Artery The splenic artery provides branches to the body and tail of the pancreas. 5 / 10 What is the anatomical position of the pancreas? A) Suprarenal Region B) Retroperitoneal C) Hypogastric Region D) Intraperitoneal The pancreas is located retroperitoneally at L1-L2 vertebral levels. 6 / 10 What is the anatomical term for the major pancreatic duct? A) Common Hepatic Duct B) Duct of Wirsung C) Duct of Santorini D) Accessory Pancreatic Duct The main pancreatic duct is also called the duct of Wirsung. 7 / 10 What is the role of the accessory pancreatic duct? A) Emulsify Fats B) Minor Papilla Drainage C) Produce Hormones D) Store Enzymes The accessory duct allows pancreatic juice to flow through the minor duodenal papilla. 8 / 10 What is the endocrine product of beta cells in the pancreas? A) Insulin B) Glucagon C) Pancreatic Polypeptide D) Somatostatin Beta cells in the Islets of Langerhans secrete insulin. 9 / 10 Which hormone stimulates the release of bile into the duodenum? A) Insulin B) Gastrin C) Secretin D) Cholecystokinin Cholecystokinin (CCK) stimulates bile release from the gallbladder. 10 / 10 What type of epithelium lines the mucosa of the gallbladder? A) Simple Cuboidal B) Pseudostratified Columnar C) Simple Columnar D) Stratified Squamous Simple columnar epithelium lines the gallbladder mucosa. Your score is The average score is 0% Description This video covers the anatomy of the bile pathway, gall bladder, and pancreas. Function of Bile: Bile contains 97% water, less than 1% bile salts, bilirubin, and fats. Emulsification of fats. Bile Pathway: Bile is produced by the liver. Biliary Ducts: Right Hepatic Duct (Ductus Hepaticus Dexter) Left Hepatic Duct (Ductus Hepaticus Sinister) Common Hepatic Duct (Ductus Hepaticus Communis) Gall Bladder (Vesica Biliaris) Cystic Duct (Ductus Cysticus) Bile Duct (Ductus Choledochus) – 7 cm long Pancreatic Duct (Ductus Pancreaticus) Hepatopancreatic Ampulla (Ampulla Hepatopancreatica) Major Duodenal Papilla (Papilla Duodeni Major) Hepatopancreatic Sphincter (Sphincter Ampullae Hepatopancreatica) – also known as the Sphincter of Oddi Gall Bladder: Fossa for the Gall Bladder (Fossa Vesicae Biliaris) Fundus of the Gall Bladder (Fundus Vesicae Biliaris) Body of the Gall Bladder (Corpus Vesicae Biliaris) Neck of the Gall Bladder (Collum Vesicae Biliaris) Wall of the Gall Bladder: Tunica Mucosa: Mucosal Folds of the Gall Bladder (Plicae Tunicae Mucosa Vesicae Biliaris) Spiral Folds (Plica Spiralis) Mucosal Glands (Glandulae Mucosae) Tunica Muscularis: Circular Muscle Fibers (Stratum Circulare) Tunica Adventitia Tunica Serosa (Part of the Hepatoduodenal Ligament) Pancreas: 14-18 cm long, 2-3 cm wide, weighing 60-100 grams. Functions of the Pancreas: Exocrine Function: Produces pancreatic juice (Succus Pancreaticus) containing digestive enzymes and bicarbonate. Endocrine Function: Releases hormones directly into the bloodstream, including insulin and glucagon. Parts of the Pancreas: Head of the Pancreas (Caput Pancreatis) Body of the Pancreas (Corpus Pancreatis) Tail of the Pancreas (Cauda Pancreatis) Topography of the Pancreas: Skeletopy: L1-L2 Holotopy: Epigastric Region, Left Hypochondriac Region Pancreatic Duct System: Main Pancreatic Duct (Ductus Pancreaticus) Accessory Pancreatic Duct (Ductus Pancreaticus Accessorius) Major Duodenal Papilla (Papilla Duodeni Major) Minor Duodenal Papilla (Papilla Duodeni Minor) Sources: Memorix Anatomy 2nd Edition by Hudák Radovan, Kachlík David, Volný Ondřej Biorender University Notes and Lectures Transcript Introduction0:03What’s up. Meditay here, and in this video, we’re gonna go through the anatomy of the Gallbladder,0:08Bile Pathway, and the Pancreas. Which are organs we call accessory organs.0:12Accessory organs are not a part of the digestive tract, but they have0:16an essential role in the actual digestion. That’s why they’re called accessory organs.0:21So, In this video, We’re first going to go through the Bile pathway, as you see here.0:25We’re gonna cover the Parts of the bile pathway, what the function of Bile essentially is,0:30and the layers of the bile duct. After that, we’ll go through the anatomy of the Gallbladder,0:35this one. Basically, talk through the different parts of it, its layers, and coverings. And then,0:41we’ll go through the anatomy of the pancreas, basically talk about its function, its topography,0:45and structures associated with it. Cool. So let’s start with the Bile pathway first.Function of Bile0:51Let’s now start by looking at an anterior view of the bile pathway. And then tilt our model a0:56little bit, so we see the entrance into the Liver. So what we see now is the Liver, gall bladder,1:03pancreas, and a perfectly drawn duodenum going around the pancreatic head as you see here.1:09So the Bile Pathways is shown here, and let’s now follow the Bile from beginning to end to really1:15see what’s going on. It all starts up here, at the Liver, because and the Liver produces the Bile.1:21Now I’m not gonna go in too much detail into the physiology of Bile since I wanna1:24focus on anatomy for now, but the Bile contains roughly around 97% water and under 1% bile salts,1:32and some slight percent of bilirubin and
Liver Anatomy
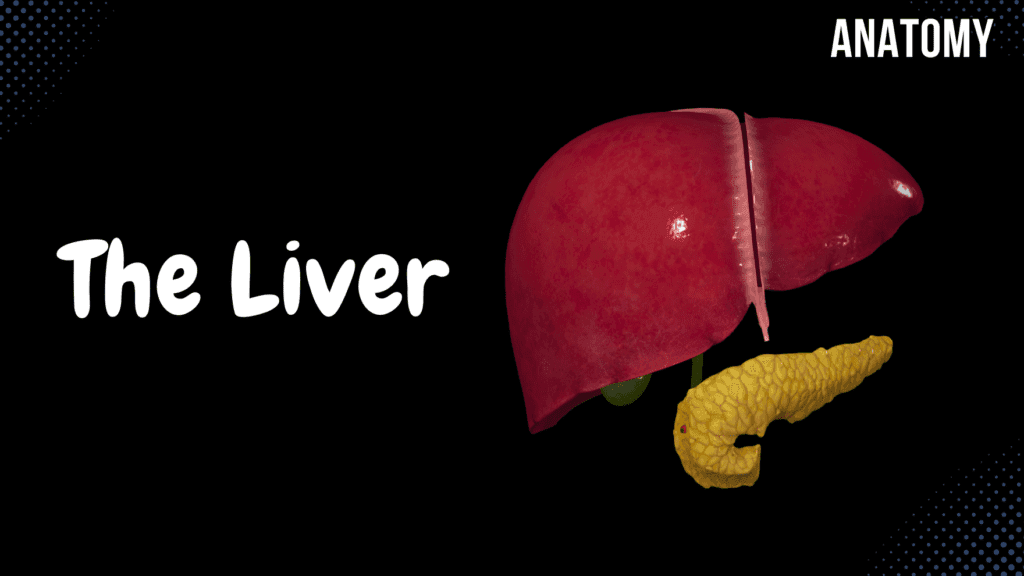
Liver Anatomy (Function, Topography, External Structures, Ligaments) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript Notes ☆ Member Only Go to PDF Notes Illustrations ☆ Member Only Go to Illustrations 12345678910 Liver – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 Which lobe of the liver is anatomically smallest? A) Left Lobe B) Quadrate Lobe C) Caudate Lobe D) Right Lobe The caudate lobe is the smallest anatomical lobe of the liver. 2 / 10 Which surface of the liver contains the bare area? A) Diaphragmatic Surface B) Visceral Surface C) Inferior Surface D) Posterior Surface The posterior surface of the liver contains the bare area. 3 / 10 What is the main digestive function of the liver? A) Glucose Storage B) Cholesterol Synthesis C) Bile Production D) Detoxification The liver produces bile, which is essential for fat digestion and absorption. 4 / 10 What structure carries bile out of the liver? A) Right Hepatic Artery B) Portal Vein C) Hepatic Vein D) Common Hepatic Duct The common hepatic duct transports bile from the liver to the bile duct. 5 / 10 What is the significance of the hepatoduodenal ligament? A) Forms Epiploic Foramen B) Suspends Liver C) Contains Coronary Ligaments D) Contains the Portal Triad The hepatoduodenal ligament encloses the portal triad (hepatic artery, portal vein, and bile duct). 6 / 10 What type of blood is carried by the hepatic artery? A) Deoxygenated Blood B) Oxygen-Poor Blood C) Oxygenated Blood D) Nutrient-Rich Blood The hepatic artery carries oxygenated blood to the liver. 7 / 10 Which region does the liver primarily occupy in the abdomen? A) Right Iliac Region B) Right Hypochondriac Region C) Left Lumbar Region D) Umbilical Region The liver is primarily located in the right hypochondriac, epigastric, and left hypochondriac regions. 8 / 10 Which veins combine to form the portal vein? A) Superior Mesenteric and Splenic Veins B) Inferior Mesenteric Vein C) Hepatic Veins D) Renal Vein The portal vein is formed by the confluence of the superior mesenteric vein and splenic vein. 9 / 10 What is the significance of the ligamentum teres? A) Hepatic Lobe Divider B) Attachment to Diaphragm C) Fetal Vein Remnant D) Lymph Node Containment The ligamentum teres is a remnant of the fetal umbilical vein, found within the falciform ligament. 10 / 10 What is the porta hepatis? A) Entry for vessels B) Hepatic Sinusoids C) Lobe Division D) Capsule of the Liver The porta hepatis is the gateway for the hepatic artery, portal vein, and bile ducts entering and leaving the liver. Your score is The average score is 0% Description Liver Function Filters blood from the digestive tract via the portal system Detoxification of harmful substances Produces bile for digestion Cholesterol synthesis Stores fat and glycogen Regulates blood sugar levels Topography of the Liver (Hepar) Holotopy: Right Hypochondriac Region, Epigastric Region, Left Hypochondriac Region Skeletopy: Superior Border: Starts at the 10th rib, extends to the 5th intercostal space at the sternum, and ends at the 6th intercostal space Inferior Border: Starts at the 10th rib, extends to the level of the 8-9th rib, and continues to the 6th intercostal space Posteriorly: T9-T11 vertebrae Syntopy: Superior Border: Diaphragmatic Surface Inferior Border (Visceral Surface): Pylorus of the stomach Colon Duodenum Right kidney Stomach Esophagus External Surface of the Liver Anterior Surface: Falciform Ligament (Ligamentum Falciforme) Right and Left Lobes Inferior Margin (Margo Inferior) Posterior Surface: Posterior Margin (Margo Posterior) Bare Area (Area Nuda) Right Sagittal Groove (Sulcus Sagittalis Dexter) Groove for Inferior Vena Cava (Sulcus Venae Cavae) Fossa for the Gallbladder (Fossa Vesicae Biliaris) Left Sagittal Groove (Sulcus Sagittalis Sinister) Round Ligament of the Liver (Ligamentum Teres Hepatis) Venous Ligament of the Liver (Ligamentum Venosum) Transverse Groove (Porta Hepatis) Division of the Liver Lobes of the Liver (Anatomical Division): Right Lobe Left Lobe Caudate Lobe Quadrate Lobe Couinaud Classification (Surgical Classification) Porta Hepatis Common Hepatic Duct Hepatic Portal Vein Proper Hepatic Artery Hepatic Plexus Hepatic Lymph Nodes Hepatoduodenal Ligament (Ligamentum Hepatoduodenale) Coverings of the Liver Tunica Fibrosa Visceral Peritoneum (Tunica Serosa) Ligaments Around the Liver Ligaments Connecting to the Diaphragm: Falciform Ligament (Ligamentum Falciforme Hepatis) Coronary Ligament (Ligamentum Coronarium Hepatis) Right Triangular Ligament (Ligamentum Triangulare Dexter) Left Triangular Ligament (Ligamentum Triangulare Sinister) Ligaments Connecting to Other Organs: Hepatogastric Ligament (Ligamentum Hepatogastricum) Hepatoduodenal Ligament (Ligamentum Hepatoduodenale) Hepatorenal Ligament (Ligamentum Hepatorenale) Round Ligament of the Liver (Ligamentum Teres Hepatis) Sources Memorix Anatomy 2nd Edition by Hudák Radovan, Kachlík David, Volný Ondřej Complete Anatomy by 3D4Medical Biorender University Notes and Lectures Transcript Introduction0:03What’s up. Meditay here, and in this video, we’re gonna go through the anatomy of the Liver.0:08So now that we’ve gone through all the digestive system structures, along with the three accessory0:13organs up here in the mouth, we’ll do the next structure, which is the Liver, since it has an0:18essential role in digestion. Our aim in this video is to understand the complete anatomy0:24and the orientation of the Liver. And to do that, We’re first going to cover the Function and the0:28Topography of the Liver. And then we’re going to look at the external structures of the Liver0:34by going through the lobes, margins, and grooves we have on the surface of the Liver,0:39and then we’re going to talk about porta Hepatis, along with how the Liver is fixated.0:43Basically, going through the covering and the ligaments you’ll find around the Liver.The Function of the Liver0:48So the Liver, or The Hepar in Latin, is the largest internal organ in the body.0:53It lies on the right side of the belly and weighs approximately 1.5 kilograms, so it’s pretty heavy.0:59The Liver’s main job is to filter the blood coming from the digestive tract before passing it to the1:05rest of the body. And it does that through the portal system. And even if you’re not familiar1:10with the portal system yet, it is quite important to understand this
Large Intestine Anatomy
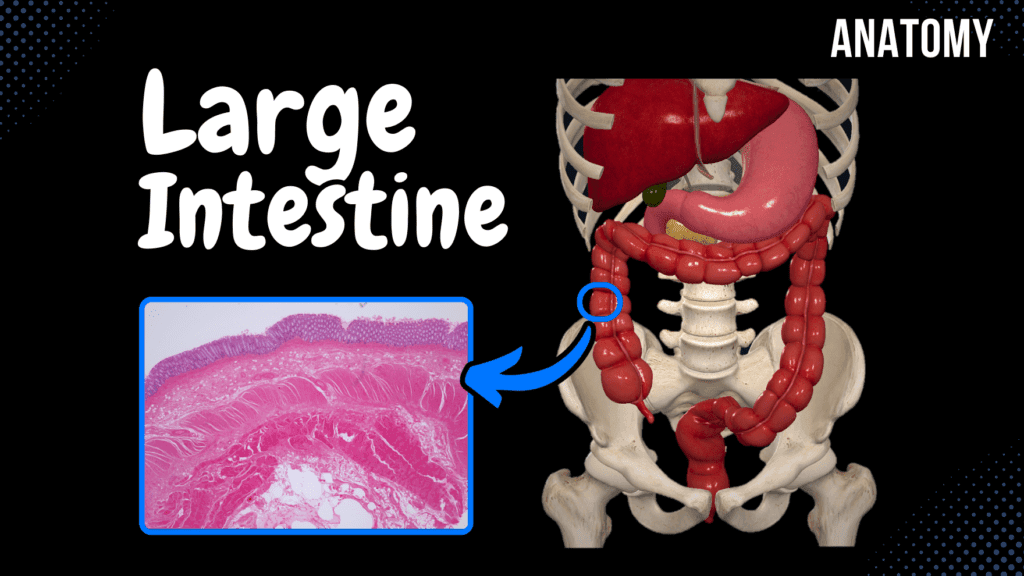
Large Intestine Anatomy (Parts, Topography, Layers) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript Notes ☆ Member Only Go to PDF Notes Illustrations ☆ Member Only Go to Illustrations 12345678910 Large Intestine – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 What is the primary blood supply to the rectum? A) Inferior Mesenteric Vein B) Superior Rectal Artery C) Middle Rectal Artery D) Inferior Rectal Artery The superior rectal artery, a branch of the inferior mesenteric artery, supplies the rectum. 2 / 10 What is the significance of the teniae coli? A) Neutralize Acid B) Aid Absorption C) Form Segmental Pouches D) Form Circular Folds Teniae coli are three longitudinal muscle bands that contract to form haustra. 3 / 10 What is the term for folds in the rectum that support fecal weight? A) Anal Columns B) Rectal Transverse Folds C) Semilunar Folds D) Haustra The rectal transverse folds (plicae transversales recti) provide structural support. 4 / 10 What is the length of the rectum? A) 10–15 cm B) 20–25 cm C) 15–20 cm D) 5–10 cm The rectum is approximately 15–20 cm long. 5 / 10 What is the function of semilunar folds in the colon? A) Transport Fats B) Store Fecal Material C) Divide Haustra D) Neutralize Acid Semilunar folds divide haustra and assist with segmentation and peristalsis. 6 / 10 What structure prevents fecal matter from re-entering the ileum? A) Rectal Sphincter B) Sigmoid Flexure C) Ileocecal Valve D) Teniae Coli The ileocecal valve prevents backflow of feces into the small intestine. 7 / 10 What structure marks the boundary between the sigmoid colon and the rectum? A) Anal Canal B) Perineal Flexure C) Sacroiliac Joint D) Rectal Ampulla The sacroiliac joint marks this transition. 8 / 10 Which layer of the large intestine contains intestinal crypts? A) Tunica Mucosa B) Tunica Serosa C) Tunica Muscularis D) Tela Submucosa Intestinal crypts are found in the tunica mucosa and house epithelial cells. 9 / 10 What is McBurney’s point associated with? A) Diverticulosis B) Intestinal Obstruction C) Hemorrhoids D) Appendicitis McBurney’s point indicates the surface location of the appendix, often used to diagnose appendicitis. 10 / 10 Which flexure separates the transverse colon from the descending colon? A) Left Colic Flexure B) Sigmoid Flexure C) Hepatic Flexure D) Right Colic Flexure The left colic flexure separates these parts of the colon. Your score is The average score is 0% Description Large Intestine Overview Latin Name: Intestinum Crassum Extends from: End of Ileum to Anus Length: 1-1.65 meters Function: Absorption of water and electrolytes Parts of the Large Intestine: Caecum Appendix Ascending Colon Transverse Colon Descending Colon Sigmoid Colon Rectum Caecum Topography: Right Inguinal Region Size: 6-8 cm long, 7-7.5 cm wide Ileal Orifice: Ostium Ileale Ileocecal Valve: Regulates flow between small and large intestine Appendix Vermiformis Size: 2-4 cm long, 0.5-1 cm wide Orifice: Ostium Appendicis Vermiformis Positions of the Appendix: Caudal Position (40-50%) Medial Position (17-20%) Lateral Position (17-20%) Posterior Position (9-13%) Anterior Position (rare) Appendicitis Inflammation of the appendix May cause peritonitis McBurney’s Point: Common site of pain T10 Dermatome: Early stage pain felt at the umbilical region Ascending Colon (Colon Ascendens) Length: 12-20 cm Topography: Right Lateral Region, Right Hypochondriac Region Syntopy: Anteriorly: Anterior Abdominal Wall Laterally: Lateral Abdominal Wall Posteriorly: Right Kidney, Quadratus Lumborum, Transverse Abdominal Muscle Transverse Colon (Colon Transversum) Length: 30-80 cm Topography: Right Colic Flexure (Flexura Coli Dextra) – Right Hypochondriac Region Umbilical Region Left Colic Flexure (Flexura Coli Sinistra) – Left Hypochondriac Region Skeletopy: L2 – L1 (Left colic flexure is higher, held by the phrenocolic ligament) Syntopy: Transverse Mesocolon, Greater Omentum Descending Colon (Colon Descendens) Length: 15-20 cm Topography: Left Lateral Region, Left Iliac Fossa Syntopy: Small Intestine, Left Kidney, Quadratus Lumborum, Abdominal Wall Ascending and Descending Colon: Mesoperitoneal Viscera (Partly covered by peritoneum) Sigmoid Colon (Colon Sigmoideum) Length: 15-80 cm Extends from: Left Iliac Fossa to the Sacroiliac Joint Continues into: Rectum Held in place by: Root of the Mesentery (Radix Mesenterii) Rectum Length: 15-20 cm Location: Anterior to Sacrum Key Structures: Sacral Flexure (Flexura Sacralis) Perineal Flexure (Flexura Perinealis) Rectal Ampulla (Ampulla Recti) Anal Canal (Canalis Analis) Anus Layers of the Large Intestinal Wall Tunica Mucosa Simple Columnar Epithelium Goblet Cells Intestinal Crypts Lamina Propria Lamina Muscularis Mucosa Semilunar Folds of the Colon (Plicae Semilunares Coli) Solitary and Aggregated Lymph Nodules Transverse Folds in Rectum: Superior Transverse Fold (Plica Transversalis Recti Superior) Middle Transverse Fold (Plica Transversalis Recti Media) Inferior Transverse Fold (Plica Transversalis Recti Inferior) Anal Structures: Anal Columns (Columnae Anales) Anal Sinuses (Sinus Anales) Tela Submucosa Loose Connective Tissue and Blood Vessels Rectal Venous Plexuses (Hemorrhoidal Plexus) – Hemorrhoidal Zone Tunica Muscularis Circular Muscle Fibers: Internal Anal Sphincter External Anal Sphincter Longitudinal Muscle Fibers: Tenia Coli: Tenia Libera (Free Tenia) Tenia Omentalis (Omental Tenia) Tenia Mesocolica (Mesocolic Tenia) Haustra of Colon (Haustrae Coli) Transverse Grooves (Sulci Transversi) Tunica Serosa Intraperitoneal Viscera Mesoperitoneal Viscera Sources: Memorix Anatomy 2nd Edition Biorender University Notes and Lectures Transcript Introduction0:03What’s up. Meditay here, and in this video, we’re gonna go through the anatomy of the0:07Large Intestine. So in the last video, we went through the anatomy of the Small Intestine.0:12Now the step after the Small Intestine is the Large Intestine, as you see here. So in0:18this video, we’re first going to go through the different parts of the large intestine,0:22as well as the topography, basically where the different parts are located in relation0:27to the surrounding structures. Then we’ll go through the layers of the large intestinal wall.Small Intestine Overview0:32So here, I’ve highlighted the large intestine or Intestinum Crassum in Latin.0:37Crassum means dense or thick. It starts at the end of the Ileum0:42and ends at the anus, so the whole colored part is the large intestine.0:47And so, if you’d stretch out the large intestine, you’d see that it would approximately be between0:531-1,5 meters long.
Small Intestine Anatomy
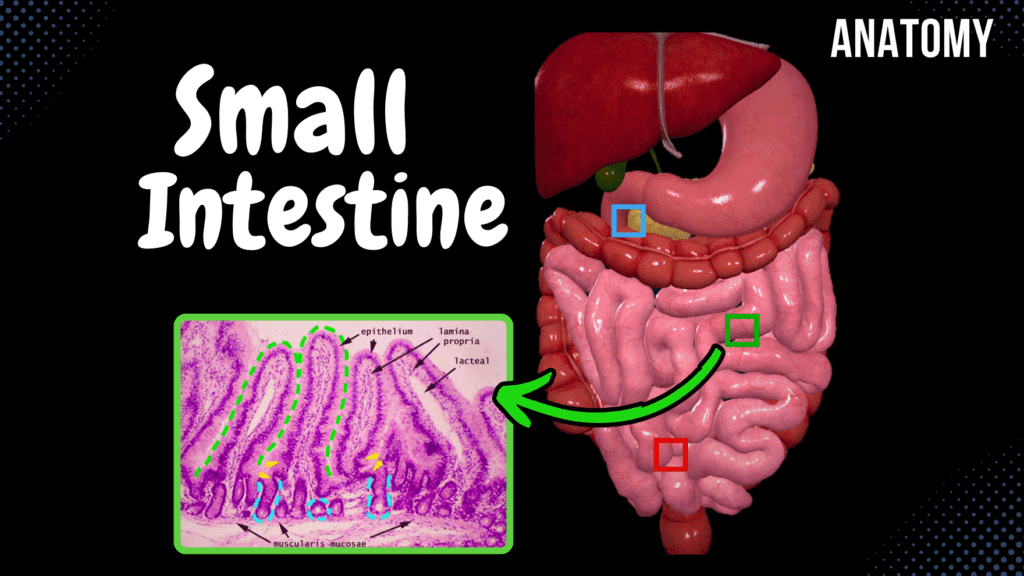
Small Intestine Anatomy (Parts, Topography, Structures, Layers) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript Notes ☆ Member Only Go to PDF Notes Illustrations ☆ Member Only Go to Illustrations 12345678910 Small Intestine – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 Which layer of the small intestine contains lymphatic vessels called lacteals? A) Tunica Mucosa B) Tela Submucosa C) Tunica Muscularis D) Tunica Serosa Lacteals are present in the villi within the tunica mucosa. 2 / 10 What is the main function of plicae circulares in the small intestine? A) Increase absorption B) Neutralize acids C) Facilitate peristalsis D) Secrete enzymes Plicae circulares increase the surface area for nutrient absorption. 3 / 10 Which region of the small intestine absorbs iron? A) Ileum B) Duodenum C) Caecum D) Jejunum Iron absorption occurs primarily in the duodenum. 4 / 10 What is the landmark where the duodenum transitions into the jejunum? A) Duodenojejunal Flexure B) Ampulla of Vater C) Minor Duodenal Papilla D) Pyloric Orifice The duodenojejunal flexure marks this transition and is supported by the ligament of Treitz. 5 / 10 Which part of the small intestine is more vascularized? A) Ileum B) Jejunum C) Colon D) Duodenum The jejunum is more vascularized, giving it a darker color compared to the ileum. 6 / 10 Which part of the small intestine is primarily intraperitoneal? A) Jejunum and Ileum B) Ileum C) Entire Small Intestine D) Duodenum The jejunum and ileum are intraperitoneal and supported by the mesentery. 7 / 10 What is the function of crypts of Lieberkühn in the small intestine? A) Absorb nutrients B) Absorb fats C) Secrete intestinal juice D) Neutralize acid These glands secrete intestinal juice and renew epithelial cells. 8 / 10 Which part of the duodenum crosses anterior to the inferior vena cava and aorta? A) Superior Part B) Horizontal Part C) Descending Part D) Ascending Part The inferior (horizontal) part of the duodenum crosses these structures. 9 / 10 Which feature of the ileum is specific for immune function? A) Plicae Circulares B) Villi C) Goblet Cells D) Peyer’s Patches Peyer’s patches are clusters of lymphoid nodules in the ileum for immune defense. 10 / 10 What structure allows bile and pancreatic secretions to enter the duodenum? A) Major Duodenal Papilla B) Minor Duodenal Papilla C) Hepatic Duct D) Ampulla of Vater The major duodenal papilla allows bile and pancreatic juices to enter the duodenum. Your score is The average score is 0% Description Anatomy of the Small Intestine Small Intestine Overview: Extends from the Pylorus to the Caecum. Approximately 7 meters long in adults. Divided into three parts: Duodenum Jejunum Ileum Duodenum: Length: 20-30 cm Functions: Iron absorption Chemical digestion Chemical neutralization Processes chyme from the stomach Topography of the Duodenum: Skeletopy: Extends from L1 to L3. Syntopy: Posteriorly: Inferior Vena Cava, Aorta, Right Kidney Superiorly: Liver, Pancreas Anteriorly: Transverse Colon Holotopy: Epigastric and Umbilical Regions Jejunum and Ileum: No clear demarcation between them. Jejunum: 2-3 meters long Primary function: Absorption Ileum: 2-4 meters long Absorbs remaining nutrients and vitamins (especially Vitamin B12). Topography of the Jejunum and Ileum: Skeletopy: L2 to Right Iliac Fossa Syntopy: Surrounded by Caecum, Ascending Colon, Transverse Colon, Descending Colon, and Sigmoid Colon. Fixated posteriorly to the abdominal wall through the Root of the Mesentery (Radix Mesenterii). Covered anteriorly by the Greater Omentum. Holotopy: Ileum: Umbilical and Left Lateral Region Jejunum: Left Lateral Region, Right Inguinal Region, Pubic Region Anatomical Structures: Duodenum: Superior Part: From Pyloric Orifice (Ostium Pyloricum) to Superior Duodenal Flexure (Flexura Duodeni Superior). Descending Part: From Superior Duodenal Flexure to Inferior Duodenal Flexure (Flexura Duodeni Inferior). Inferior Horizontal Part: From Inferior Duodenal Flexure. Ascending Part: Until Duodenojejunal Flexure (Flexura Duodenojejunalis) / Ligament of Treitz. Jejunum: Wider and thicker than the ileum. More vascular. Darker in color. Ileum: Thinner walls. Less vascular. Lighter in color. Layers of the Small Intestinal Wall: Tunica Mucosa: Simple Columnar Epithelium Circular Folds (Plicae Circulare) – Absent in the Duodenal Bulb Intestinal Villi (Villi Intestinales) Microvilli Intestinal Glands (Glandulae Intestinales) Solitary Lymphoid Nodules (Noduli Lymphoidei Solitarii) Aggregated Lymphoid Nodules (Noduli Lymphoidei Aggregati) Specialized Structures in Duodenum: Major Duodenal Papilla (Papilla Duodeni Major) Minor Duodenal Papilla (Papilla Duodeni Minor) Tela Submucosa: Duodenum: Contains Brunner’s Glands. Jejunum: Longer villi. Ileum: More goblet cells and Peyer’s Patches (GALT). Tunica Muscularis: Responsible for Peristaltic Movement Inner Layer: Circular Muscle Layer Hepatopancreatic Sphincter (Sphincter of Oddi) (M. Sphincter Ampullae Hepatopancreatica) Outer Layer: Longitudinal Muscle Layer Tunica Serosa: Intraperitoneal Organs: Covered by Peritoneum. Retroperitoneal Organs (e.g., Duodenum): Have Tunica Adventitia in certain areas. Sources: Memorix Anatomy, 2nd Edition by Hudák Radovan, Kachlík David, and Volný Ondřej Biorender University Notes and Lectures Transcript Introduction0:04What’s up. Meditay here, and in this video, we’re gonna go through the anatomy of the0:08Small Intestine. So in the last video, we went through the anatomy of the Stomach.0:12Now the step after the Stomach is the Small Intestine, as you see here. So in this video,0:18we’re first going to look at the components that make up the small intestine, then we’re going0:23to look at their topography and go through how the small intestine is fixated to the posterior0:28abdominal wall. After that, we’ll look at some important anatomical structures related to the0:34three parts of it. And then, we’ll go through the layers that make up the small intestinal wall.Small Intestine Overview0:40Alright, so here you see the anterior view of the abdominal cavity,0:44the whole small intestine is highlighted in blue here.0:47It reaches from the Stomach all the way to the large intestine, as you see here.0:52To be more specific, it goes from the pylorus of the Stomach to the caecum of the large intestine.0:58Now the length of the small intestine may vary, but in total, if you stretch it out,1:04it’d be approximately 7 meters long. Let’s now look at the parts of the small1:08intestine to get a
Stomach Anatomy
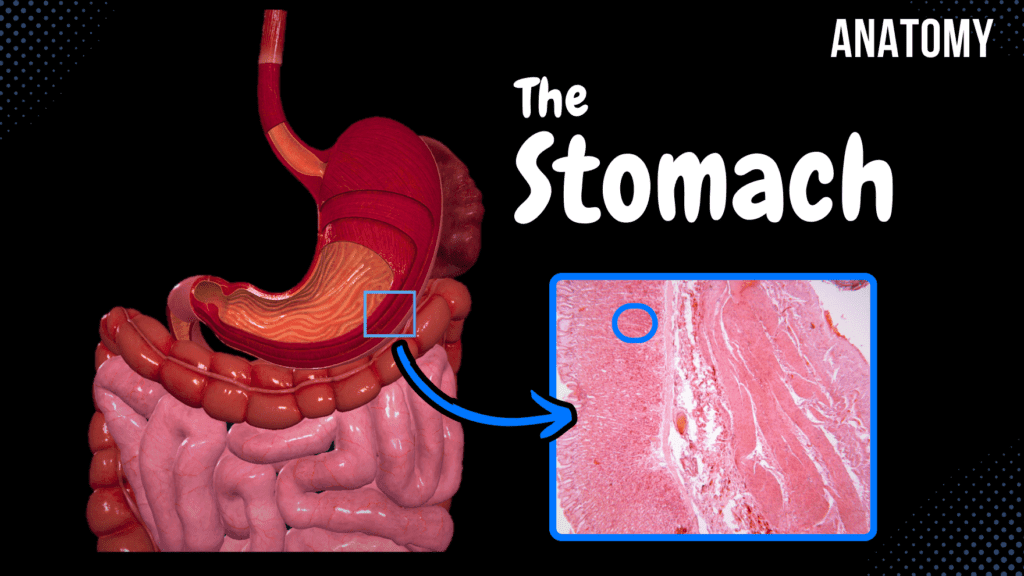
Stomach Anatomy (Topography, External Features, Parts, Layers) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript Notes ☆ Member Only Go to PDF Notes Illustrations ☆ Member Only Go to Illustrations 12345678910 Stomach – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 Which ligament contains the portal triad? A) Hepatogastric Ligament B) Hepatoduodenal Ligament C) Gastrosplenic Ligament D) Gastrocolic Ligament The hepatoduodenal ligament encloses the portal vein, hepatic artery, and bile duct. 2 / 10 Which part of the stomach transitions into the duodenum? A) Fundus B) Cardiac Part C) Pyloric Part D) Body The pyloric part transitions into the small intestine via the pyloric canal and sphincter. 3 / 10 Which ligament forms part of the greater omentum and attaches the stomach to the diaphragm? A) Gastrophrenic Ligament B) Gastrosplenic Ligament C) Hepatogastric Ligament D) Gastrocolic Ligament The gastrophrenic ligament connects the stomach to the diaphragm. 4 / 10 What is the role of parietal cells in the stomach? A) Mucus B) HCl and Intrinsic Factor C) Hormones D) Pepsinogen Parietal cells secrete hydrochloric acid (HCl) and intrinsic factor. 5 / 10 What is the main venous drainage of the greater curvature of the stomach? A) Gastric Veins B) Splenic Veins C) Gastro-omental Veins D) Short Gastric Veins The gastro-omental veins drain the greater curvature. 6 / 10 What is the primary parasympathetic innervation of the stomach? A) Hypoglossal Nerve B) Sympathetic Chain C) Vagus Nerve D) Splanchnic Nerve The vagus nerve provides parasympathetic innervation to the stomach. 7 / 10 Which stomach wall layer facilitates peristaltic movement? A) Tunica Serosa B) Tela Submucosa C) Tunica Muscularis D) Tunica Mucosa The tunica muscularis, with its three muscle layers, facilitates peristalsis. 8 / 10 What is the term for the narrowing of the pyloric canal due to hypertrophy in infants? A) Achalasia B) Gastritis C) Gastric Ulcer D) Pyloric Stenosis Pyloric stenosis involves hypertrophy of the pyloric muscle, leading to narrowing. 9 / 10 What is the significance of the areae gastricae in the stomach? A) Secretes enzymes B) Protects the mucosa C) Provides blood supply D) Increases surface area Areae gastricae are small elevations of mucosa that increase the stomach’s absorptive surface. 10 / 10 Which ligament anchors the lesser curvature of the stomach to the liver? A) Gastrosplenic Ligament B) Gastrocolic Ligament C) Hepatogastric Ligament D) Gastrophrenic Ligament The hepatogastric ligament is part of the lesser omentum and connects the stomach to the liver. Your score is The average score is 0% Description Anatomy of the Stomach Topography of Gaster: Holotopy: Located in the Epigastric Region and Left Hypochondriac Region (Left Upper Quadrant). Extends from the Cardiac Orifice (Ostium Cardiacum) to the Pyloric Orifice (Ostium Pyloricum). Syntopy (Relations to Neighboring Structures): Anterior Wall: Diaphragm, Liver, Anterior Abdominal Wall Posterior Wall: Left Kidney, Spleen, Pancreas, Transverse Colon External Features of the Stomach: Lesser Curvature (Curvatura Minor) Angular Notch (Incisura Angularis) Greater Curvature (Curvatura Major) Cardiac Notch (Incisura Cardialis) Parts of the Stomach: Cardiac Part (Pars Cardiaca) Fundus (Fundus Gastricus) Body (Corpus Gastricum) Pyloric Part (Pars Pylorica) Pyloric Antrum (Antrum Pyloricum) Pyloric Canal (Canalis Pyloricus) Layers of the Gastric Wall: Tunica Mucosa (2-3 mm thick) Gastric Folds (Plicae Gastricae) Gastric Areas (Areae Gastricae) Simple Columnar Epithelium Gastric Pits (Foveolae Gastricae) Lamina Propria Muscularis Mucosae Tela Submucosa Loose connective tissue Tunica Muscularis (Smooth Muscle Layers) Inner: Oblique Muscle Layer Middle: Circular Muscle Layer Pyloric Sphincter (Musculus Sphincter Pyloricus) Outer: Longitudinal Muscle Layer Tunica Serosa Formed by the peritoneum Sources: Memorix Anatomy, 2nd Edition by Hudák Radovan, Kachlík David, and Volný Ondřej Biorender University Notes and Lectures Transcript Introduction0:00What’s up. Meditay here, and in this video, we’re gonna go through the anatomy of the stomach.0:04So in the last video, we went through the anatomy of the Esophagus. Now the step after0:09the Esophagus is the Stomach, as you see here. So in this video, we’re first going to go through0:14the topography of the stomach, basically where it is related to surrounding structures. After that,0:21we’re going to look at the external features of the stomach and the different parts of it. Then0:26we’ll go through the layers of the gastric wall. Now. Let’s go ahead and start with the topography.Topography of the Stomach0:31So the stomach lies in the epigastric region and the left hypochondriac region, as you see here.0:36Or, if you’re studying using the 4 quadrant division,0:38you’ll find it in the left upper quadrant. If we expose the stomach a little more,0:44you’ll see that it starts from the abdominal part of the Esophagus,0:48and then it curves to the left and then reaches out to the small intestine.0:53And these two openings that go towards the Esophagus and the small intestine has unique names0:59The opening by which the Esophagus communicates with the stomach is known as the cardiac orifice1:06at the level of the 10th to 11th thoracic vertebrae. And the opening by which the1:11stomach communicates with the duodenum of the small intestine is known as the pyloric orifice1:16at the level of the 1st lumbar vertebra So if we look at the stomach from this1:21perspective, laterally, you’ll see this. The stomach has an Anterior wall and a1:27Posterior wall. So from this position, we can look at the1:30Syntopy, meaning the position of the Stomach To other organs. Anteriorly1:36We can find the Diaphragm being very close to the anterior wall; we’ll find the liver,1:41and we’ll also find the stomach facing the anterior abdominal wall aswell. And the1:46Posterior wall of the Stomach is close to the left kidney. You’ll also see the spleen,1:51the pancreas, and the transverse colon facing the posterior surface of the stomach as well.External Features of the Stomach1:56So that was the Syntopy. Now, let’s go back and look at the external structures of the stomach.2:01We can see two distinct curvatures; we have the lesser curvature2:06Here. And since we have a lesser curvature, we also have a greater curvature here. On the2:11lesser curvature,
How to Divide the Abdomen
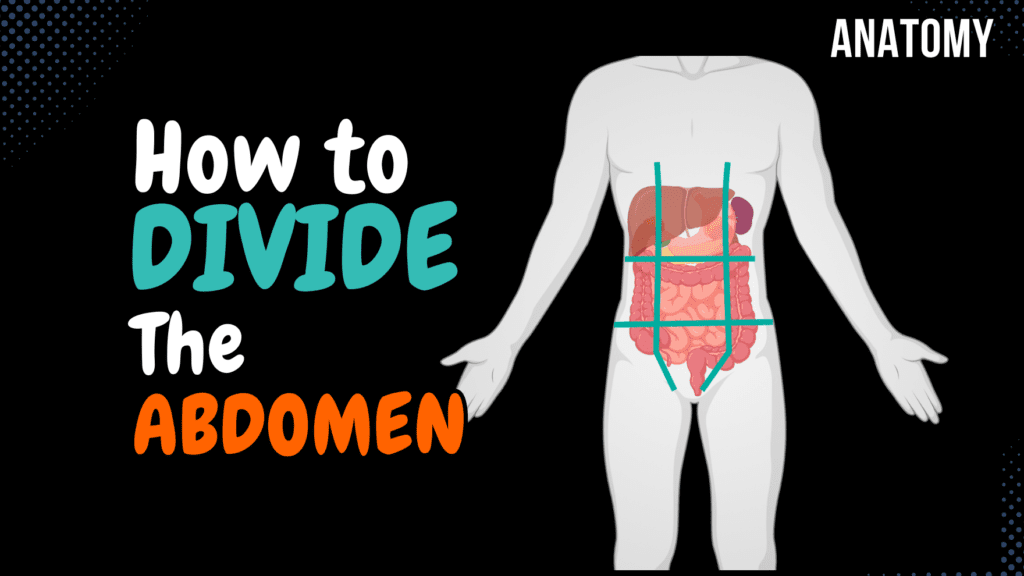
How to Divide the Abdomen (9 Regions) Official Links Instagram Youtube Jki-discord Notes & Illustrations Quizzes Summary & Transcript 📢 Currently, there is no PDF for this video.If you’re interested in having one, feel free to send an inquiry, and I may create it in the future. BUT! There’s a quiz available in the next tab. 12345678910 Dividing the Abdomen – QUIZ Test your understanding with 10 random multiple-choice questions from the question bank. You're in the preview mode. Note: All elements work correctly on the front end. 1 / 10 Which region lies inferior to the epigastric region in the nine-region scheme? A) Hypochondriac Region B) Inguinal Region C) Umbilical Region D) Pubic Region The umbilical region lies directly inferior to the epigastric region. 2 / 10 Which region is located at the center of the nine abdominal regions? A) Right Hypochondriac Region B) Epigastric Region C) Umbilical Region D) Pubic Region The umbilical region is located at the center of the nine abdominal regions. 3 / 10 What region contains most of the small intestine? A) Right Lateral Region B) Pubic Region C) Umbilical Region D) Epigastric Region The umbilical region contains most of the small intestine. 4 / 10 What is the distance between the ribs used for abdominal division called? A) Distantia Costarum B) Costal Angle C) Rib Separation D) Subcostal Width The distance is called distantia costarum. 5 / 10 What is the function of the interspinal plane in abdominal division? A) Identify Organs B) Separate Middle and Lower Levels C) Divide Quadrants D) Aid Vascular Mapping The interspinal plane separates the middle and lower levels of the abdomen. 6 / 10 Which organ is primarily located in the pubic region? A) Small Intestine B) Bladder C) Liver D) Appendix The bladder is the primary organ in the pubic region. 7 / 10 What anatomical landmark is used for the vertical lines in abdominal division? A) Sternum B) Iliac Crest C) Rectus Abdominis and Clavicle D) Umbilicus The vertical lines follow the rectus abdominis muscle and pass through the midpoint of the clavicle. 8 / 10 What is the name of the lower horizontal plane? A) Subcostal Plane B) Interclavicular Plane C) Interspinal Plane D) Suprapubic Plane The interspinal plane is the lower horizontal plane used in abdominal division. 9 / 10 Which vertical lines are used in the nine-region scheme? A) Sagittal Lines B) Intercostal Lines C) Subclavicular Lines D) Midclavicular Lines The vertical lines pass through the midpoint of the clavicle and the pubic tubercle. 10 / 10 What is the anatomical name for the vertical lines in the four-quadrant scheme? A) Transumbilical Line B) Midclavicular Line C) Median Plane D) Sagittal Line The vertical line is called the median plane. Your score is The average score is 0% Description Dividing the Abdominal Region This video covers how the abdominal region is divided using anatomical planes and regions. Holotopy: The relation between an organ and the body as a whole. Horizontal Lines: Upper Horizontal Plane: Subcostal Plane Lower Horizontal Plane: Interspinal Plane Distance between the ribs: Distantia Costarum Divided into: Upper Level Middle Level Lower Level Vertical Lines: Along the Rectus Abdominis Muscle From the Pubic Tubercle (Tuberculum Pubicum) Extends approximately to the middle point of the clavicle 9-Region Scheme: Upper Level: Epigastric Region Right Hypochondriac Region Left Hypochondriac Region Middle Level: Umbilical Region Right Lateral (Lumbar) Region Left Lateral (Lumbar) Region Lower Level: Pubic (Hypogastric) Region Right Inguinal Region Left Inguinal Region 4-Quadrant Scheme: The abdomen can also be divided into four quadrants: Right Upper Quadrant (RUQ) Left Upper Quadrant (LUQ) Right Lower Quadrant (RLQ) Left Lower Quadrant (LLQ) Why Divide the Abdomen? Used in clinical practice to locate pain and pathology. Helps in understanding the placement of abdominal organs. Essential for surgical and diagnostic procedures. Sources: Memorix Anatomy, 2nd Edition by Hudák Radovan, Kachlík David, and Volný Ondřej Biorender University Notes and Lectures Transcript Introduction0:03What’s up, Meditay here, and in this video, we’ll be going through the procedure on how0:08we divide the abdomen into 9 distinct regions. Because as you’re studying the organs of the0:13abdominal cavity, you’ll most probably see the word Holotopy, which means the relationship0:18between the organs and the body as a whole, and by describing the holotopy of an organ, you’ll0:23be stating at which region the organ Is located. So, Let’s start by dividing the abdominal regionHorizontal Lines0:29using two horizontal lines first. We call these the Upper horizontal plane, and the0:34lower horizontal plane. The upper horizontal plane is at the lowest point of the costal arch and is0:40therefore also called the subcostal place. While the lower horizontal plane is between the Spina0:46Iliaca ant. Superior, so the lower horizontal place is sometimes called the interspinal plane.0:53This will divide the abdomen into three levels using this arch0:56Right here that the lower edges of the rib cartilage form, that’s the distance between1:00the ribs – called distantia costarum. Now We get an upper level, above this arch,1:06We get a middle level under the costal arch, until the1:09Interspinous place, and then under the interspinous plane, you’ll find the lower level.Vertical Lines1:15And now, we need to add the vertical lines. And we add them using the rectus1:20Abdominis muscle, as you see here. And the way we add the vertical lines is along this muscle,1:25along the Musculus rectus abdominis. It starts Down here at pubic tubercule1:30Then it goes along the rectus abdominis and then reaches approximately at the1:34middle point of the clavicula up here. So now we get nine distinct regions, right?Nine Regions1:40At the upper level, we get the epigastric region and the Right and Left hypochondriac region on1:45either side beneath the cartilage. And then on the middle level, we get1:48the umbilical region in the middle, since the umbilicus, or the navel, is here in the middle.1:53And then, laterally, we have the right and left lateral region.1:57And then, at the lower region, we got the pubic region and the right and left inguinal2:02region or sometimes also referred to as the right and left Iliac
